- Home
- Provider Administrative newsletter
- September 2019
September 2019
Featured Story: Coming soon - submit medical specialty drug requests online
We're excited to announce a new way to obtain medical specialty drug prior authorization. From the AllWays Health Partners provider portal, you will have direct access to submit your medical specialty drug requests online through the NovoLogix prior authorization system - no additional registration or login required!
In this Issue
- Coming soon: submit medical specialty drug requests online
- Reminder: HPV vaccine covered for all members through 45
- Behavioral health for children and adolescents
- Antidepressant adherence
- Drug fee schedules to be updated
- Medical policy
- Code updates and reminders
- Contact Information
Coming soon: submit medical specialty drug requests online through NovoLogix
We're excited to announce a new way to obtain medical specialty drug prior authorization. From the AllWays Health Partners provider portal, you will have direct access to submit your medical specialty drug requests online through the NovoLogix prior authorization system - no additional registration or login required!
Online submission gives you the most efficient way to get your requests processed. Once submitted, you will have instant access to real-time status updates.
For those who prefer to fax in your requests, you may continue to fax these requests to NovoLogix at 844-851-0882.
Stay tuned for more information.
As more information becomes available, we'll share updates with you. If you are not yet registered for the AllWays Health Partners provider portal, sign-up today. For support with the provider portal registration process, email us at prweb@allwayshealth.org or call 855-444-4647. We are available Monday through Friday, 8 AM to 6 PM.
Register for the provider portal.
Reminder: HPV vaccine covered for all members through 45
According to the Centers for Disease Control (CDC), every year about 14 million Americans become infected with Human Papillomavirus (HPV). HPV viruses are associated with several forms of cancers. To help combat the spread of HPV-related diseases and cancers, AllWays Health Partners recently extended coverage for the HPV vaccine through the age of 45 for all our members.
For more information, we recently shared some best billing practices for immunizations in our provider blog.
Behavioral health for children and adolescents
AllWays Health Partners regularly reviews and updates our coverage for behavioral health services. We recently updated our commercial coverage for children and adolescents. Here's an overview of some of the behavioral health services we cover for children and adolescents up to age 19.
For questions about coverage or help finding a contracted provider, contact Optum at 844-451-3520 (Partners HealthCare plan members) or 844-451-3518 (all other commercial members).
Antidepressant adherence
Depression is one of the most common conditions in behavioral health, and it has a significant impact on both mental and physical well-being. After an initial diagnosis of depression is made, a primary care provider may consider starting a patient on an antidepressant medication for treatment of his/her illness.
AllWays Health Partners in collaboration with its Behavioral Health vendor, Optum, has been working on a variety of initiatives to raise awareness about the objectives of National Committee for Quality Assurance (NCQA) HEDIS® Antidepressant Medication Management (AMM) measures, which guide our efforts in measuring the quality and effectiveness of the care provided.
To learn more about the AMM measure and best practices to improve the measure, check out a recent post in our provider blog.
Identifying depression in PCP setting
Drug fee schedules to be updated
AllWays Health Partners reviews its drug fee schedules quarterly to ensure that they are current, comprehensive and consistent with industry standards, to the extent supported by its systems. In most cases, changes involve adding fees for new or existing codes, to supplement the fees already on the fee schedule.
The next update will occur on October 1, 2019. Changes may involve both new and existing CPT and HCPCS codes, and will include the planned quarterly update to physician administered drugs, immune globulin, vaccine and toxoid fees.
Medical policy
The following medical policy updates are effective September 1, 2019:
- Absorbent Products - Annual update. References updated.
- Oral and Maxillofacial Surgery and Procedures - Annual update. Revised oral appliances exclusion to allow for treatment of OSA. Updated references.
- Outpatient Drug Screening and Testing - Annual update. References updated.
Code Updates and Requirements
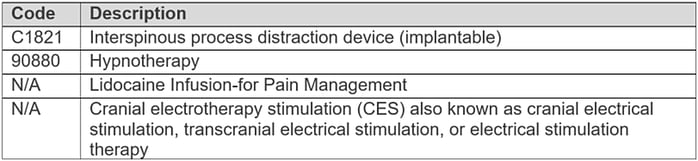
The following services are not covered as they are considered experimental/ investigational, effective 11/1/19:
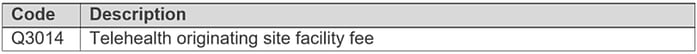
The following service is covered but not separately reimbursable, effective 9/1/19:
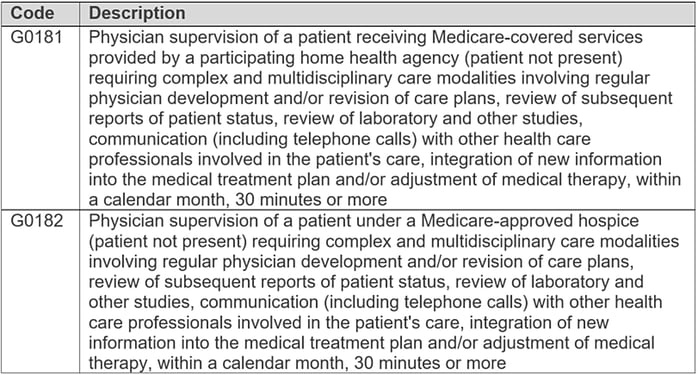
The following services are covered, effective 9/1/19:
The following drugs are covered with prior authorization, effective 10/1/19:
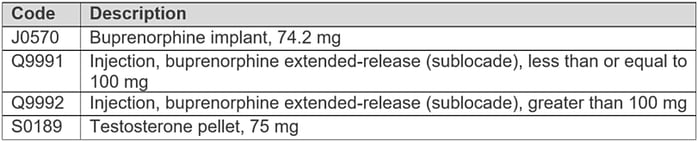
Note: Suboxone film is covered without prior authorization for MassHealth members.
Insulin Pumps
For all lines of business, the prior authorization requirement for outpatient insulin pumps has been lifted.
Preventative Services
- Preventative diabetes screening - For all lines of business, the frequency limit on preventative diabetes screening has been lifted as of 7/3/19.
- Preventative healthy diet counseling - The minimum age restriction on preventative healthy diet counseling has been removed as of 1/1/19.
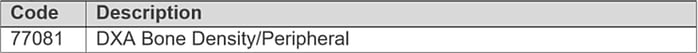
- Preventative osteoporosis screening – The following code is covered under the preventative osteoporosis screening benefit when billed with a preventative diagnosis, effective 1/1/19: