Claims information
Payer ID numbers and addresses for submitting medical and behavioral health claims.
How to use this page
To ensure accurate submissions of your claims, answer these three questions:
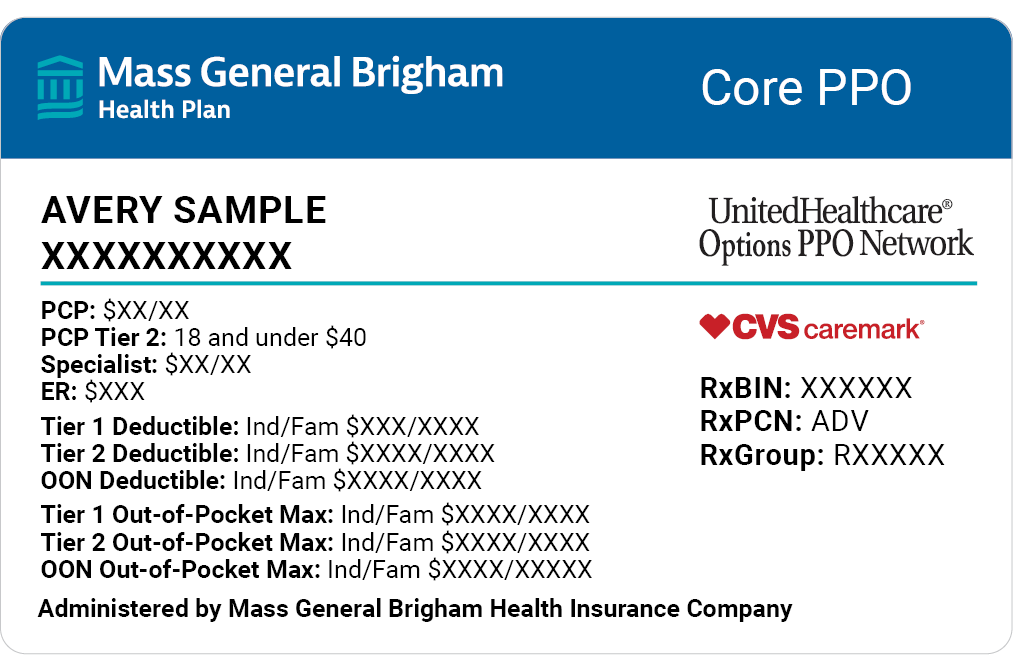
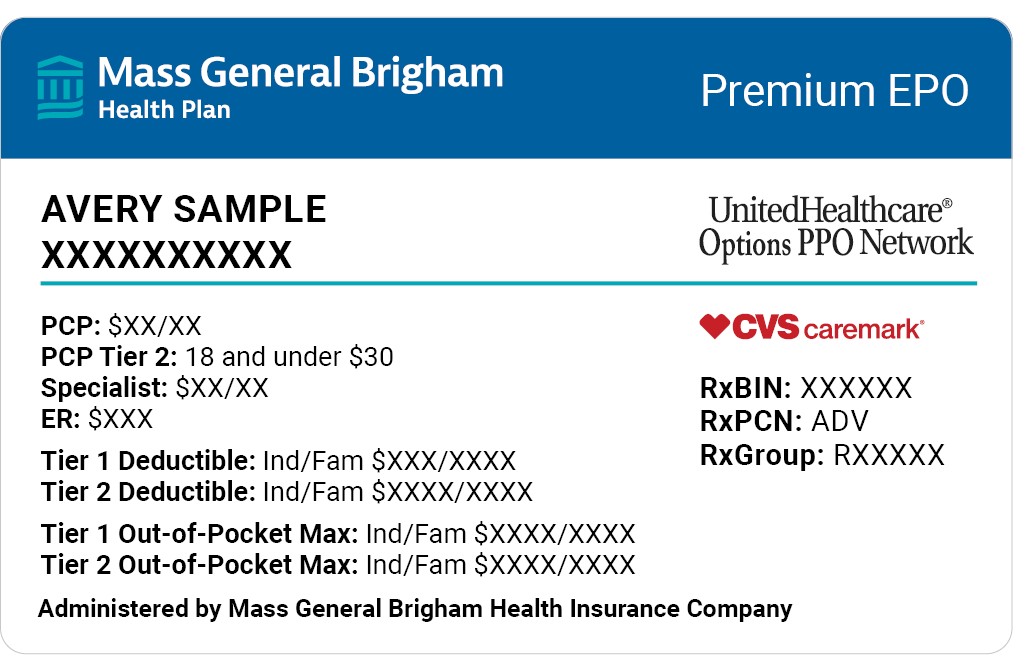
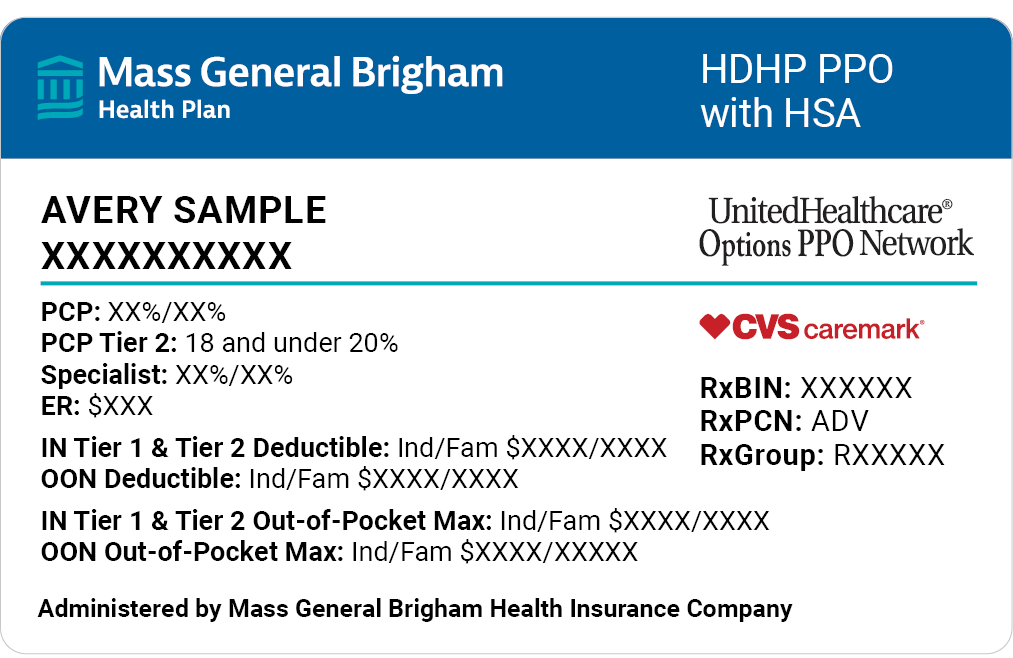
- What plan is it? Mass General Brigham plans have instructions specific to them.
- What type of plan is it? Check the section on HMO plans & PPO Plus plans for instructions specific to those plan types.
- What state are you located in? Your state will help determine where you should submit your claims.
Additional claims resources
Here you'll find additional resources and forms related to the Mass General Brigham Health Plan claims processes.
Mass General Brigham Health Plan network providers in all states and non-contracted providers in Massachusetts should submit claims directly to Mass General Brigham Health Plan.
Mass General Brigham Health Plan
Provider Service: 855-444-4647
Payer ID: 04293
Paper Claims: PO Box #323, Glen Burnie, MD 21060
Non-contracted providers outside of Massachusetts should submit claims to UnitedHealthcare Shared Services.
UnitedHealthcare Shared Services
Visit https://uhss.umr.com or 866-683-6441
Payer ID: 39026, Group ID: 78800271
Paper Claims: P.O. Box 30783, Salt Lake City, UT 84130-0783
All behavioral health providers should submit claims to Optum.
Optum provider Service: 844-451-3520
Payer ID: 87726
Paper Claims: PO Box 30757, Salt Lake City, UT 84130-0757
Visit the Optum Provider Express Portal for more information and to check member eligibility. When checking eligibility for Mass General Brigham Health Plan members, remember to search by name and date of birth.
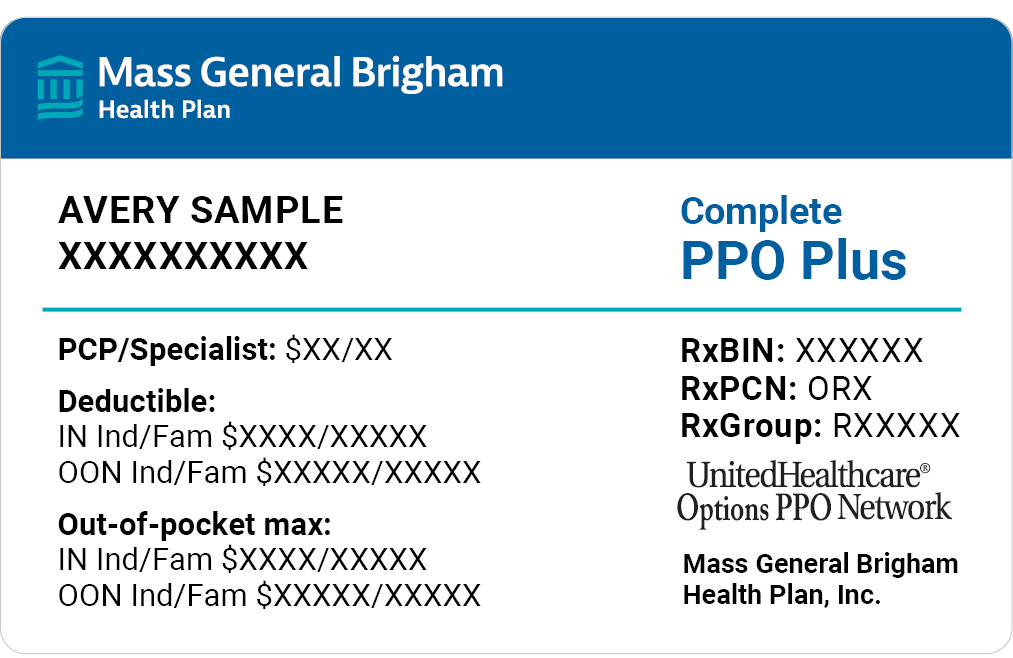
HMO plans & PPO Plus plans
HMO plans include access to the Mass General Brigham Health Plan network. PPO Plus plans include access to the UnitedHealthcare Options PPO network.
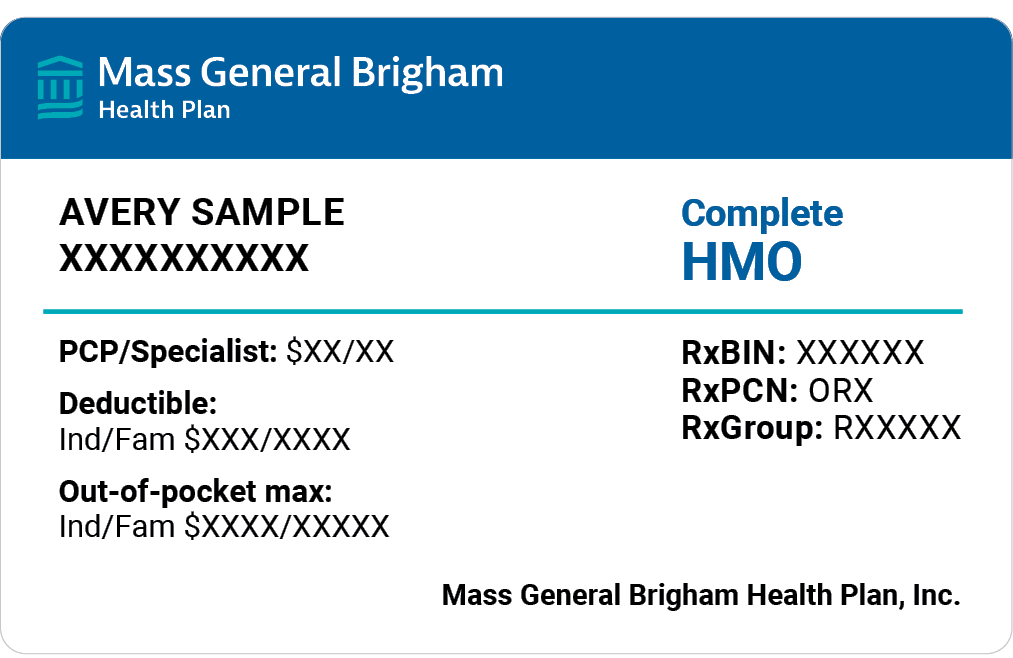
HMO plans:
Providers contracted with Mass General Brigham Health Plan and non-contracted providers in Massachusetts, New Hampshire, and Rhode Island:
Mass General Brigham Health Plan
Provider Service: 855-444-4647
Payer ID: 04293
Paper Claims: PO Box #323, Glen Burnie, MD 21060
Urgent and emergency care outside of Massachusetts, New Hampshire, and Rhode Island:
UnitedHealthcare Shared Services
Visit https://uhss.umr.com or 866-683-6441
Payer ID: 39026, Group ID: 78800215
Paper Claims: P.O. Box 30783, Salt Lake City, UT 84130-0783
PPO Plus plans:
Providers in Massachusetts and New Hampshire:
Mass General Brigham Health Plan
Provider Service: 855-444-4647
Payer ID: 04293
Paper Claims: PO Box #323, Glen Burnie, MD 21060
Providers outside of Massachusetts and New Hampshire:
UnitedHealthcare Shared Services
Visit https://uhss.umr.com or 866-683-6441
Payer ID: 39026, Group ID: 78800215
Paper Claims: P.O. Box 30783, Salt Lake City, UT 84130-0783
Submit behavioral health claims to Optum.
Provider Service: 844-451-3518
Payer ID: 87726
Paper Claims: PO Box 30757, Salt Lake City, UT 84130-0757
Visit the Optum Provider Express Portal for more information and to check member eligibility. When checking eligibility for Mass General Brigham Health Plan members, remember to search by name and date of birth.
Complete Access EPO plans
Complete Access EPO members in MA and NH have access to the Mass General Brigham Health Plan network, and members outside MA/NH can seek care from the UnitedHealthcare Options PPO network.
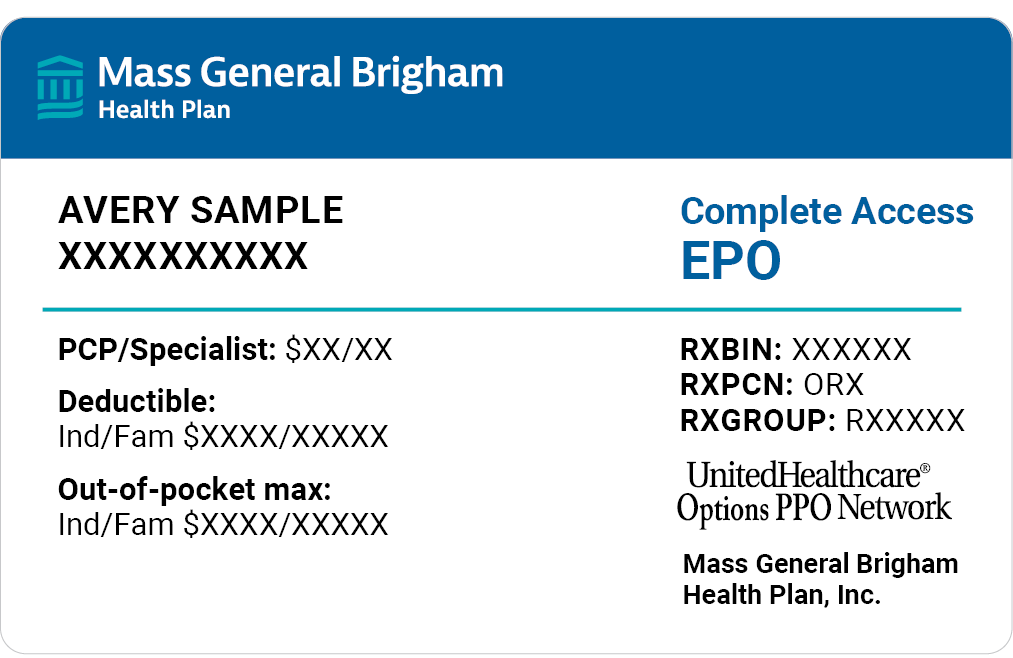
Providers in MA & NH:
Mass General Brigham Health Plan
Provider Service: 855-444-4647
Payer ID: 04293
Paper Claims: P.O. Box #323 Glen Burnie, MD 21060
Providers outside MA & NH:
UnitedHealthcare Shared Services
Visit uhss.umr.com or call 866-683-6441
Payer ID: 39026
Group ID: 78800215
Paper Claims: P.O. Box 30783, Salt Lake City, UT 84130-0783
Submit behavioral health claims to Optum.
Optum
Provider Service: 844-451-3518
Payer ID: 87726
Paper Claims: P.O. Box 30757, Salt Lake City, UT 84130-0757
Mass General Brigham ACO plans
Mass General Brigham Health Plan is proud to provide MassHealth insurance coverage to members of Mass General Brigham ACO.
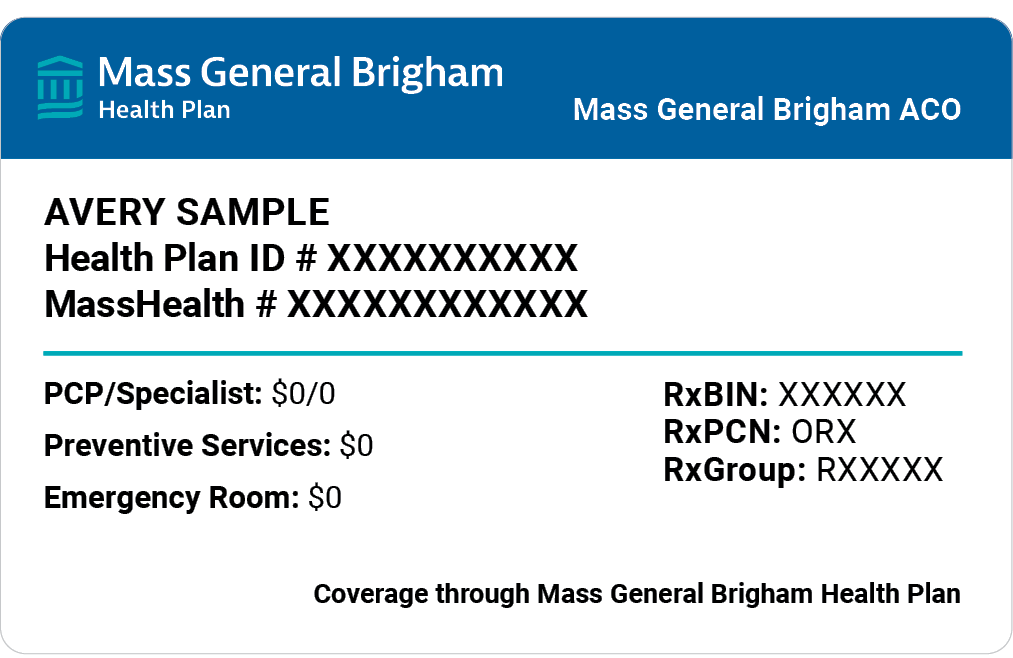
Mass General Brigham Health Plan billing information:
Mass General Brigham Health Plan Provider Service: 855-444-4647
Payer ID: 04293
Paper Claims: PO Box #323 Glen Burnie, MD 21060
Submit behavioral health claims to Optum.
Provider Service: 844-451-3519
Payer ID: 87726
Paper Claims: P.O. Box 30760, Salt Lake City, UT 84130-0760
Visit the Optum Provider Express Portal for more information and to check member eligibility.
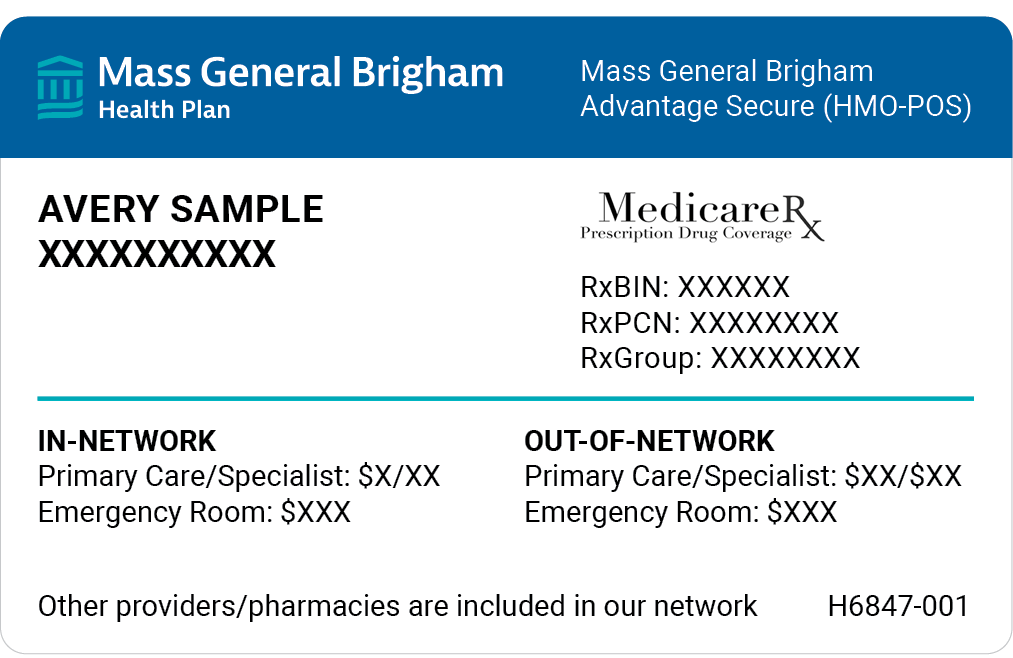
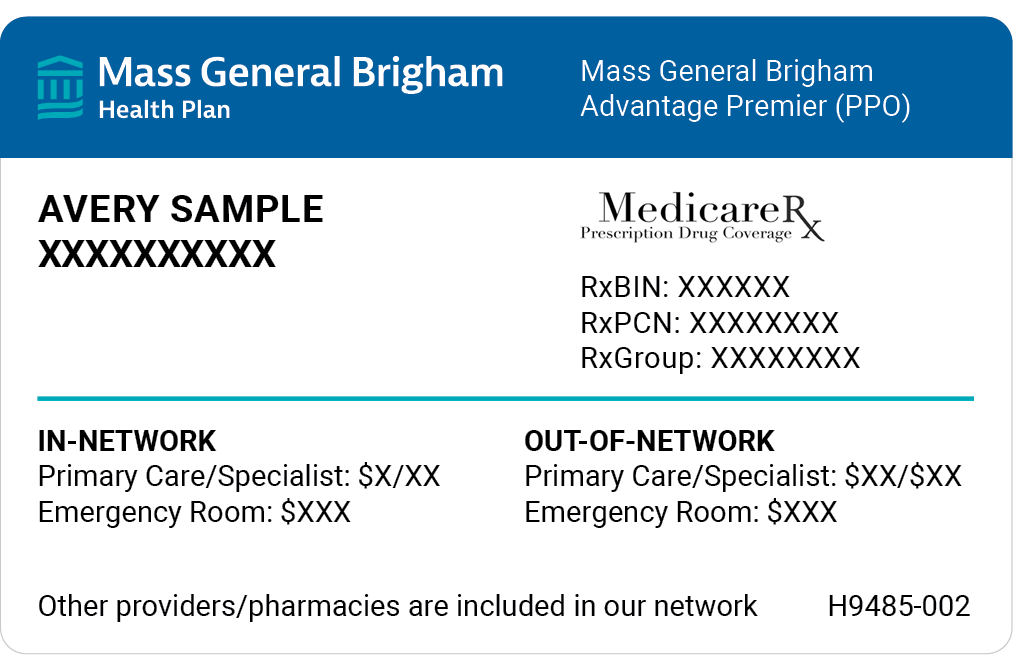
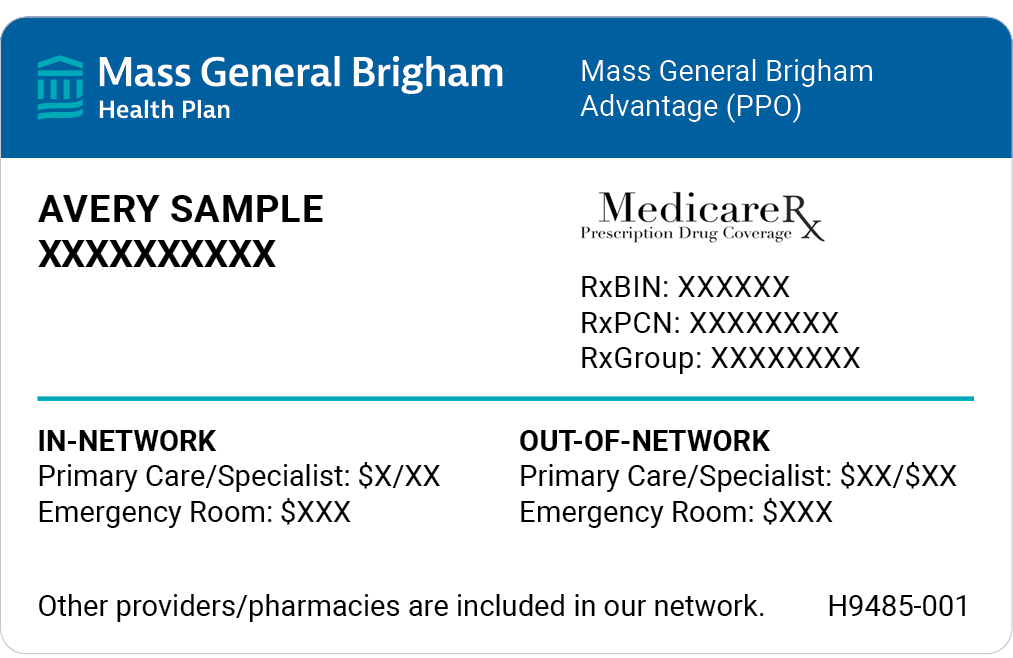
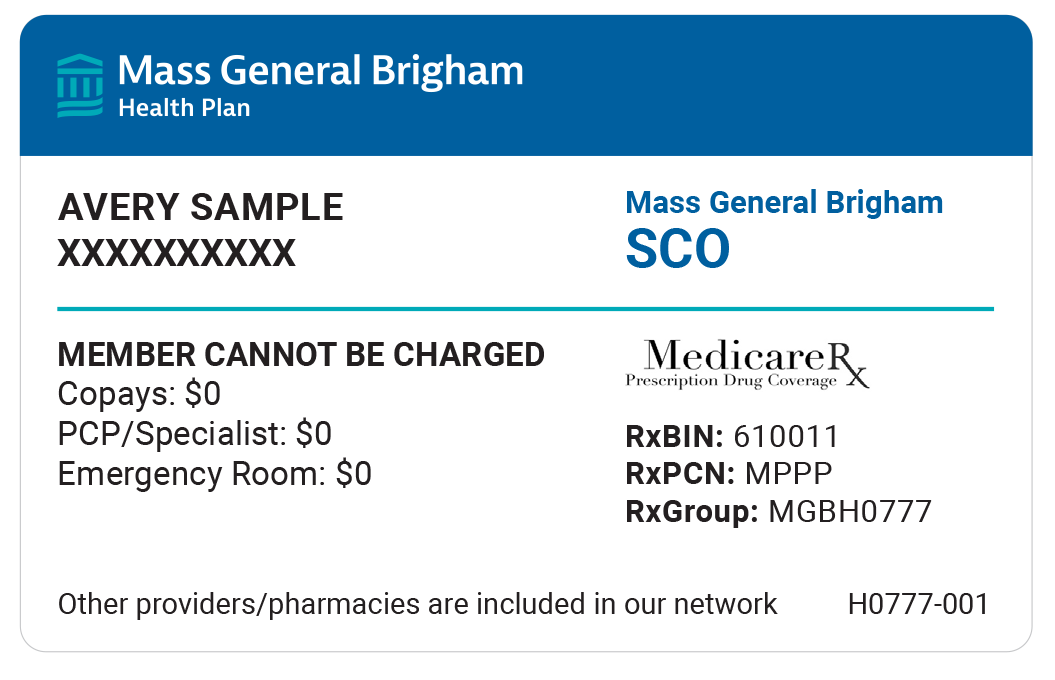
Medicare Advantage plans
Medicare Advantage is a bundled plan option that adds additional coverage to Original Medicare. Original Medicare (Parts A and B) includes hospital insurance for both inpatient and home health, and medical insurance for doctor visits and some preventive care. Medicare Advantage (Part C) plans combine Part A, Part B, and often Part D (drug coverage), to provide members with full-coverage benefits including dental, vision, hearing, and more.

Medicare Balance plans
Medicare Balance provides secondary coverage to Medicare — all members are required to have both Medicare Parts A and B. Medicare Balance does not have a provider network, so members may choose to see any doctor, anywhere in the nation, who accepts Medicare. Medicare Balance members don't need a referral to see a specialist.
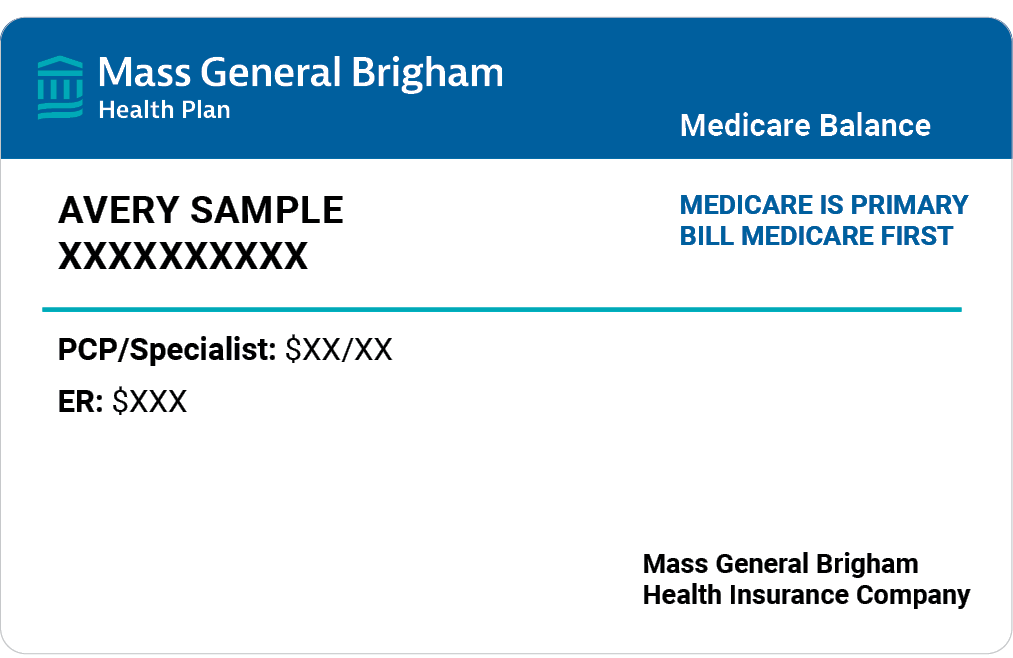
Claims information
For billing purposes, Medicare should be listed as the member's primary coverage and Medicare Balance as their secondary coverage. Also, Medicare Balance pays the entire balance on member deductibles and coinsurance costs for services charged at the Medicare-allowed amount. So, you don't have to collect any out-of-pocket fees from your patients.
Mass General Brigham Health Plan billing information:
Mass General Brigham Health Plan Provider Service: 855-444-4647
Payer ID: 04293
Paper Claims: 399 Revolution Drive, Somerville, MA 02145 Suite 875
Submit behavioral health claims to Optum.
Optum
Provider Service: 866-262-8067
Payer ID: 87726
Paper Claims: P.O. Box 30757, Salt Lake City, UT 84130-0757
Mass General Brigham Health Plan billing information:
Mass General Brigham Health Plan Provider Service: 855-444-4647
Payer ID: 04293
Paper Claims: 399 Revolution Drive, Somerville, MA 02145 Suite 875
Submit behavioral health claims to Optum.
Optum
Provider Service: 866-262-8067
Payer ID: 87726
Paper Claims: P.O. Box 30757, Salt Lake City, UT 84130-0757

Need to check the status of a claim?
You can check claims and eligibility 24/7 on our secure provider portal.