- Home
- Provider Administrative newsletter
- November 2019
November 2019
Featured Story: Remember to use the provider portal for member eligibility and claims status
The provider portal gives you instant and real-time access to validate member eligibility and check on claims status. Beginning January 1, we will direct all phone calls to verify member eligibility or check on claims status to the provider portal. This will give you a faster response time for urgent inquiries that requires support from provider service staff.
In this Issue
- Reminder: use the provider portal for member eligibility and claims status
- Behavioral Health Quality assurance toolkit for PCPs
- Quick tips: authorizations in a closed status
- Formulary updates
- HEDIS data collection
- Medical policy
- Code updates and reminders
- Contact Information
Reminder: use the provider portal for member eligibility and claims status
The provider portal gives you instant and real-time access to validate member eligibility and check on claims status. Beginning January 1, we will direct all phone calls to verify member eligibility or check on claims status to the provider portal. This will give you a faster response time for urgent inquiries that requires support from provider service staff.
Please share this important information with your staff and with third-party billers who call us on your behalf.
Registering for the provider portal
Getting setup with the provider portal is easy. Here are useful resources to help you get started today:
For registration support, contact prweb@allwayshealth.org.
Register for the provider portal.
Behavioral health quality assurance toolkit for PCPs
What is the Quality Assurance Toolkit?
The Quality Assurance Toolkit (QA Toolkit) was designed with busy providers in mind. It's an informational guide that explains what each HEDIS® measure is, how to achieve success in meeting the measure, what PCPs need to know about various behavioral health conditions, and recommended treatment options. By monitoring the percentage of a set of patients that meet the goal for a measure and developing processes to help improve this percentage, it is hoped that the overall health of the patients will improve.
Learn more about it at: https://www.providerexpress.com/content/ope-provexpr/us/en/clinical-resources/quality-assurance-toolkit.html
Why is Quality Assurance Important?
- QA standards helps providers confidently address the needs of patients with behavioral health needs
- Improvement in QA measures generally produces better outcomes for patients
- QA scoring help patients, providers and health plans assess the overall quality of care being provided
What is HEDIS?
Healthcare Effectiveness Data and Information Set (HEDIS) is a set of standardized performance measures designed to ensure that purchasers and consumers have the information they need to reliably compare the performance of managed health care plans.
There are HEDIS measures for both behavioral health and physical health conditions. Examples for physical health include: Immunizations, Diabetes, Mammography, Cholesterol, High Blood Pressure, etc. Examples for behavioral health include: Antidepressant Medication Management, Follow-Up After Hospitalization for Mental Illness, Diabetes Screening for People with Schizophrenia or Bipolar Disorder Who Are Using Antipsychotic Medications, Initial and Engagement of Alcohol and Drug Treatment.
Quick tips: authorizations in a closed status
As a reminder, the provider portal gives you real-time status updates on authorizations and referrals. Its important to always check that the appropriate authorizations or referrals are approved before the service.
When viewing the authorization, the overall authorization status can be found in the Authorization/Referral Status box:
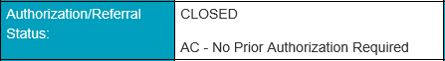
Closed Authorizations
Authorizations in a closed status cannot be revised. If the intended service is still needed, has not yet occurred and requires prior authorization, please submit a new request.
Reasons for authorizations being closed
There are many reasons for an authorization to be closed. Here’s a look at some common reasons:- Prior authorization is not required for the requested service.
- The wrong service on the form was selected (example: an outpatient request was submitted on the inpatient request form). Resubmit and select the appropriate service form.
- There is an existing authorization that should be revised instead of creating a new request.
- The service is managed by a vendor (example: eviCore, Optum, CVS Caremark). Submit the request with the appropriate vendor.
- The authorization was moved to a newborn baby ID number.
- The request is a duplicate authorization.
- The request was entered in error.
- The service is no longer needed.
- AllWays Health Partners is the secondary insurance. Authorization is not required.
- The service requires both a referral and a prior authorization. Contact the member’s primary care provider to obtain the referral.
Visit our website to access authorization and referral submission user guides, requirements and process information.
Formulary updates
AllWays Health Partners regularly reviews and updates our formulary to ensure alignment with the industry. Check out the latest updates effective January 1, 2020.
For the latest information on our pharmacy programs, visit our online formulary today.
HEDIS data collection
The Healthcare Effectiveness Data and Information Set (HEDIS®) is a widely-used standardized set of performance measures developed and maintained by the National Committee for Quality Assurance (NCQA). HEDIS was designed to help consumers compare health plan performance to other plans and to national or regional benchmarks.
Each year, NCQA requires health plans to collect and report HEDIS data from contracted providers. HEDIS data collection will run from January 2020 through the end of May 2020. A member of AllWays Health Partners' HEDIS staff will ask you to fax, mail, submit by FTP the information or schedule an onsite review at your location.
Based on the HEDIS measures, PCPs and a subset of specialties such as OB/GYN, cardiology, ophthalmology, and optometry are the most likely to receive a medical records request.
We appreciate your cooperation and timely response during this review and thank you in advance.
For more information, view the HEDIS FAQ
Contact Us
- Call: 857-282-7403
- Email: HEDIS@allwayshealth.org
- Fax: 617-526-1931
Medical policy
The following medical policy updates are effective November 1, 2019:
- Luxturna - Annual update. References updated.
- Therapeutic Lens - Annual review. References updated. Added Post-operative cataract extraction (limited to one set of contact lens per surgery) as a medical condition under conventional contact lens.
- Corneal Collagen Cross-linking - Annual review. References updated.
- Macimorelin (Macrilen®) - Macimorelin is a growth hormone (GH) secretagogue receptor agonist indicated for the diagnosis of adult growth hormone deficiency (AGHD).
Code updates and reminders
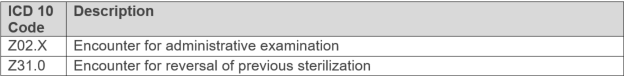
As a reminder, the following diagnoses are not covered across all lines of business:
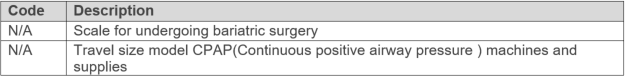
As a reminder, the following services are not covered across all lines of business:
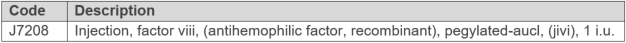
The following drugs are covered under the medical benefit with prior authorization:
The following drugs are covered under the medical benefit without prior authorization:
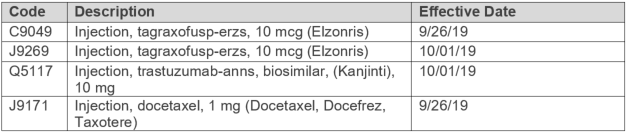
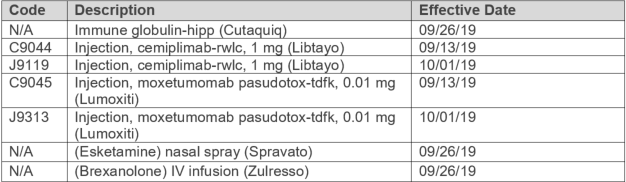
October Codes
The following codes are not covered as they are considered experimental/investigational, effective 10/1/19:
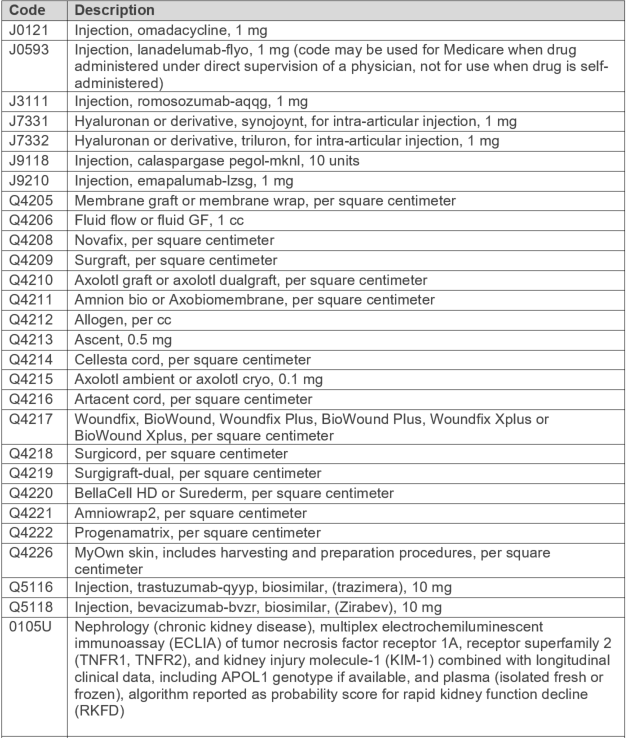
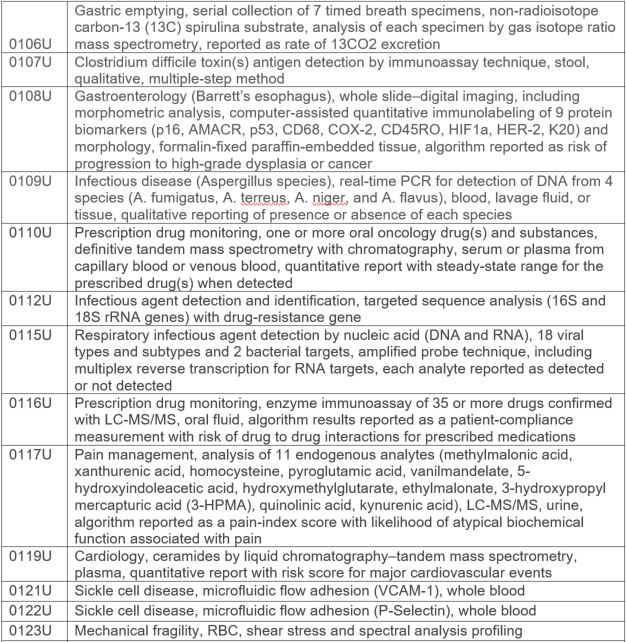
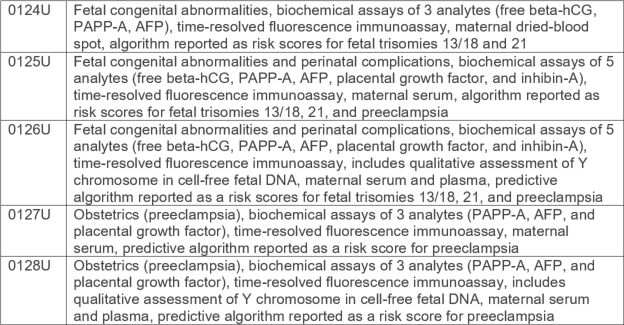
The following codes are covered; no prior authorization required, effective 10/1/19:
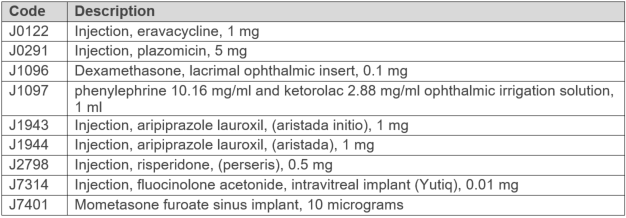
The following codes are covered with prior authorization, effective 10/1/19:
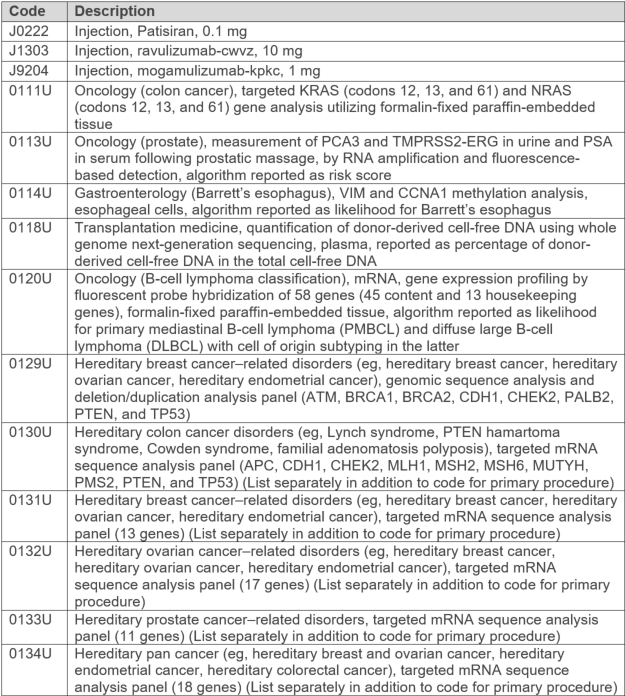
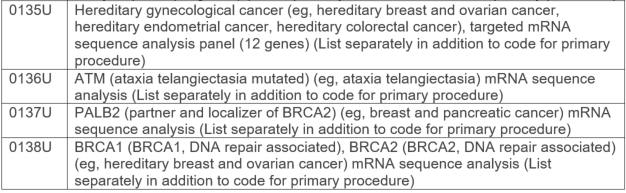
The following codes are not payable; reportable only; effective 10/1/19:
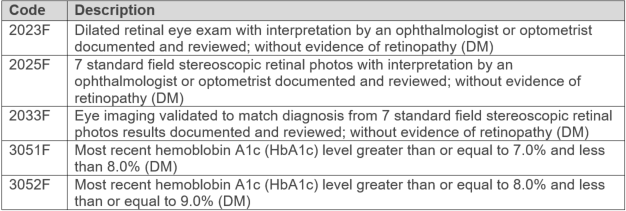
The following code is not covered for Commercial; Covered with prior authorization for My Care Family, effective 1/1/20:
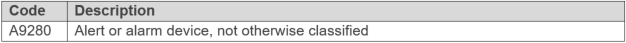
The following codes are covered but not payable, effective 1/1/20:

The following code is not reimbursable for My Care Family, effective 1/1/20:
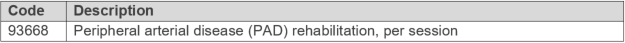
The following service is not covered as it is considered experimental/investigational:
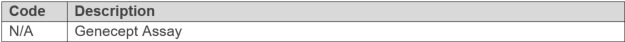
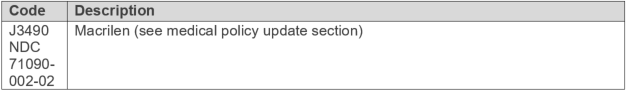
The following drug is covered with prior authorization, effective 11/1/19:
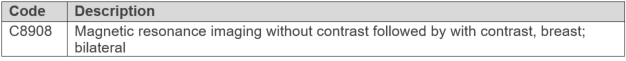
Breast MRI
Effective 10/1/19, the following HCPCS code is recognized for coverage and payment for MRI of the breast:
Drug Coverage
Effective 8/29/19, the following code is covered with prior authorization: