- Home
- Provider Administrative newsletter
- Everything you need to know in January 2021
Everything you need to know in January 2021
Featured story: COVID-19 updates
Our COVID-19 FAQs for providers give you the latest information, updates and resources. We are constantly updating our commercial and MassHealth FAQs as more information becomes available from the Federal and State governments. Please check back periodically to get the most recent news.
In this issue:
- COVID-19 updates
- Notification of Birth (NOB) Process
- Annual Provider Meeting & Product trainings
- New Products Webinar
- E/M code updates
- Reminders
- CPT Code Updates
- Medical Policy Updates
- Quarterly Hospital Admission Report
COVID-19 updates
Take a look at the latest COVID-19 updates as of January 1, 2021.
Lab test U0003 – U0005
In alignment with the Centers for Medicare and Medicaid Services, which serves as a basis for AllWays Health Partners rate development, as of January 1, 2021, we have lowered the base payment amount for COVID-19 diagnostic tests run on high-throughput technology. In addition, we will make an additional add-on payment to laboratories for a COVID-19 diagnostic test run on high throughput technology if the laboratory:
- Completes the test in two calendar days or less AND
- Completes the majority of their COVID-19 diagnostic tests that use high throughput technology in two calendar days or less for all their patients (not just their Medicare patients) in the previous month
For complete information, visit our COVID-19 FAQ. Please note that U0005 must be billed on the same claim as U0003 or U0004. It cannot be billed as a stand-alone procedure.
Telemedicine cost sharing
To ensure continued access to care, we have removed cost sharing (copayments, deductibles, or coinsurance) for medically necessary COVID-19 telemedicine visits. As of January 1, 2021, cost sharing will resume for non-COVID-19-related telemedicine visits with PCPs, specialists, and additional providers, such as urgent and routine care, and outpatient behavioral health services.
Notification of Birth (NOB) Process
As of 1/1/2021, MassHealth will have a new NOB process and electronic form. You can see an at-a-glance grid of the changes here.
Overview of changes for all newborns as of 1/1/21
- Babies will no longer be automatically assigned to their mother’s plan.
- Hospitals will be required to notify MassHealth within 10 days of a baby’s birth whenever possible.
- There are two new fields on the NOB form so the family can select a plan and PCP.
- Babies will be enrolled in MassHealth fee-for-service until MassHealth receives the NOB and assigns a plan.
- To determine eligibility and plan information, hospitals should check the MassHealth electronic verification system daily.
For further details please refer to the MassHealth Bulletin.
Annual Provider Meeting & Product Trainings
Don’t forget to RSVP for our annual provider meeting on Thursday, January 14, 2021 at 12 PM. This year, the meeting will be held via Microsoft Teams, and we’ll cover topics like:
- Our 2021 product portfolio
- Prior authorization tools and resources
- The latest COVID-19 updates
During the meeting, you’ll also have the opportunity to submit questions and hear from Christine Murphy, Vice President of Network Management.
New Products Webinar
Join us and learn about our new product Allies HMO, where members have access to a dedicated health navigator, quicker appointment times for select specialties, and enhanced virtual care.
You'll also learn about Select HMO, where members have access to comprehensive benefits at a lower cost through a network of high-quality providers.
Sign up now for one of the three training sessions below:
- Friday 1/29/21 - 12PM - 1PM
- Wednesday 2/3/21 - 10AM - 11AM
- Friday 2/12/21 - 12PM - 1 PM
E/M code updates
Evaluation and Management Code updates
In 2021, the AMA and CMS will implement significant changes to office/outpatient evaluation and management (E/M) visit coding and payment. The changes will reduce the documentation requirements for the history and exam components and put the emphasis on the level of medical decision making (MDM) and time spent with the patient.
- Physicians will have the option to select the level of code using either total time or level of medical decision-making
- The definition of total time will expand to include all time spent in the care of the patient (face-to-face and nonface-to-face) on the date of the encounter.
- Criteria for medical decision-making levels will be updated
- The patient history and physical exam elements will be eliminated as components of E/M code level selection
- Code 99201 will be deleted, effective 1/1/21
Reminders
Verify member eligibility and claims status
Remember to verify eligibility prior to the service to ensure you have the latest coverage information. The provider portal gives you real-time access to validate this information in seconds. As of January 1, all phone calls to verify member eligibility or check claims status are directed to the provider portal.
Confirm your Provider Directory information
To ensure that your patients and prospective patients have access to the correct information for your practice, it is important to regularly validate your practice information in our Provider Directory and let us know when an update is needed.
Remember to review information such as: contact information (telephone, fax, email), addresses, website information, network participation status, availability to see new patients, and which individual providers work at each practice location.
You can submit a provider information update request 24/7 through our secure Provider Portal or by submitting the Standardized Provider Information Change Form to pec@allwayshealth.org.
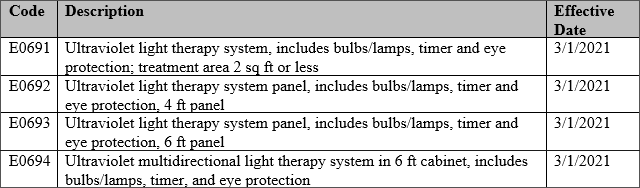
CPT Code Updates
As a reminder to our network the following services are not covered across all lines of business:
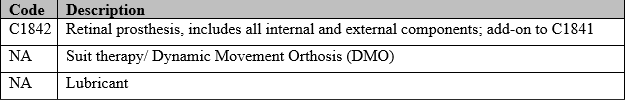
As a reminder to our network the following service is covered but not separately reimbursable across all lines of business:
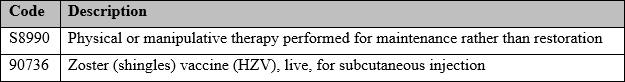
As a reminder to our network the following codes are covered with no prior authorization for MassHealth only:
The following codes are not covered experimental and investigational for all lines of business:
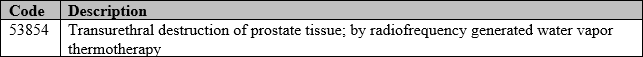
The following codes are covered with prior authorization for all lines of business:
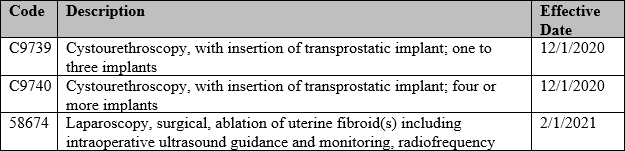
The following codes are covered with prior authorization for Commercial lines of business:
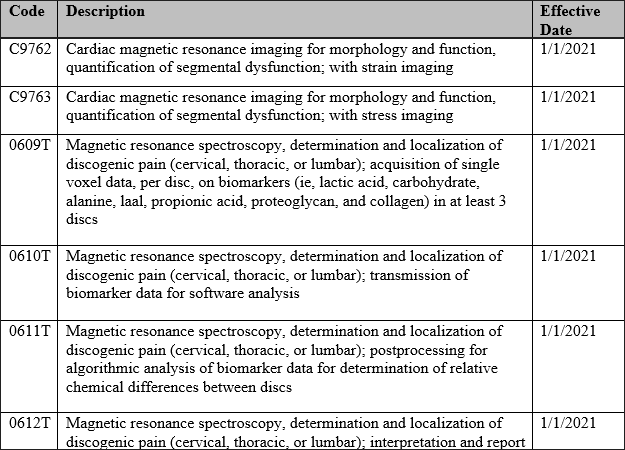
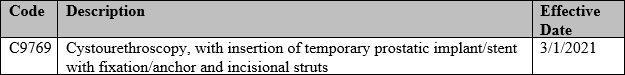
The following codes are covered with no prior authorization for commercial and ASO only:
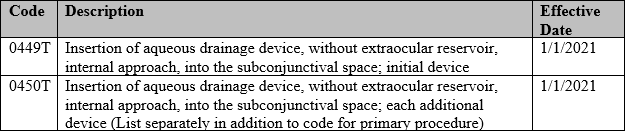
The following codes are not covered per benefit for MassHealth:
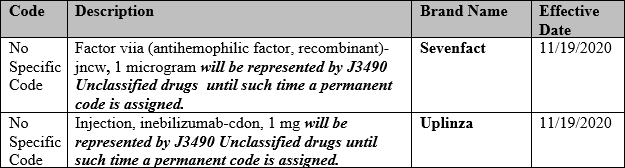
Drug Code Updates
The following drug(s) are covered under the medical benefit; no prior authorization:
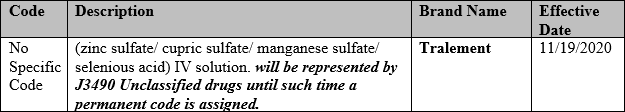
The following drug(s) are covered under the medical benefit; prior authorization required:
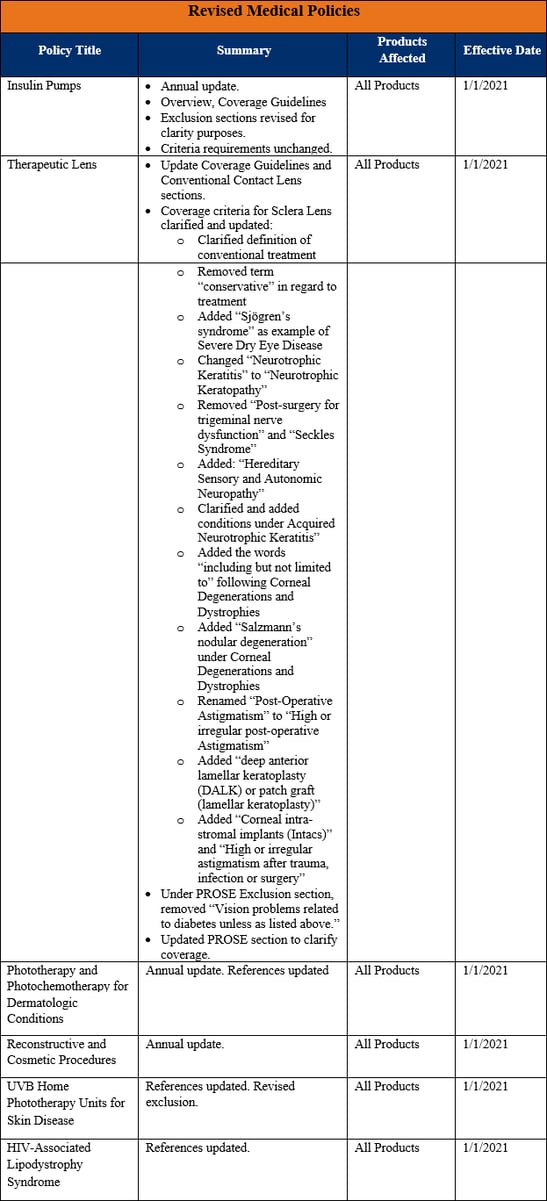
Medical Policy Updates
Quarterly Hospital Admission Report
The latest quarterly hospital inpatient utilization report is now available. To review this report, click on the Reports tab in the Provider Portal and select Clinical Reports. If you do not have access to the Provider Portal, you may register online at allwaysprovider.org.
