- Home
- Provider Administrative newsletter
- Provider Monthly: The all-new AllWays member app, an upcoming webinar, and important reminders for providers in June 2021
Provider Monthly: The all-new AllWays member app, an upcoming webinar, and important reminders for providers in June 2021
As you probably noticed from our email, they way we're sharing our newsletter has a new look and feel based on your feedback. If you'd like to share your thoughts on on similar items in the future, join our online advisory group today.
Featured Story:
Do your patients know about the all-new AllWays member mobile app?
Now, your patients can manage their healthcare on the go with our all-new AllWays member mobile app. The easy-to-use app simplifies searching for providers, accessing plan information, and contacting our customer support team. To learn about all the features designed to improve your patients' healthcare experience, visit allwayshealthpartners.org/memberapp
In this issue:
- Upcoming webinar: new authorization process for high-tech and cardiac imaging
- Message from the Pharmacy Team
- New member search tool
- Revised medical policies
- Code updates
Upcoming webinar: new authorization process for high-tech and cardiac imaging
EviCore will no longer process prior authorization requests for high-tech radiology or cardiac imaging. After July 18, you must use the authorization tool in our provider portal to request approval for these services. On June 23 at 12pm EST we will be hosting a webinar to train providers on the upcoming changes. Save your spot below:
Message from the Pharmacy Team
The state of Massachusetts requires all medication prior authorization requests to be completed using the Massachusetts Standard Form (MAPA) for medication prior authorization requests. Submission of incomplete MAPA forms or submission of any form other than the MAPA, may result in denials and delays in therapy. To ensure your submission is complete,- Attach all relevant info: definitive diagnosis with CPT/ICD-10
- Attach treatment history, including dates and source of prior treatments and outcomes
- Attach current and historical clinical notes and laboratory data/reports supportive of the request: (TB, Genotype, Fibroscan, etc.) or other test results as required by criteria
- Sign and date all requests
All of our pharmacy and medical specialty criteria are readily available on our website for providers to see what the criteria is for the specific medication.
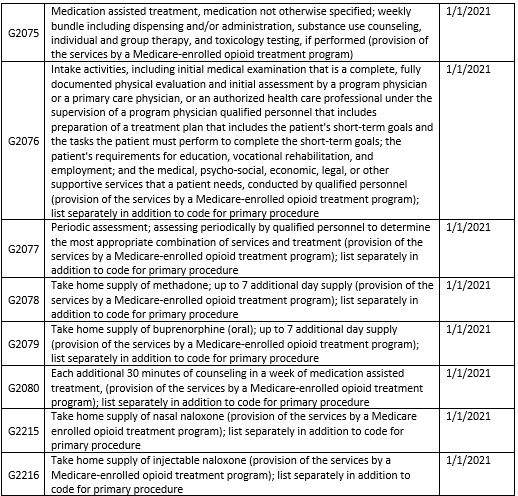
New member search tool
We’ve added extra authentication factors for added security within our member search tool. Now, you’ll be required to fill out additional field such as Member ID and Last Name to search eligibility. See screenshot below: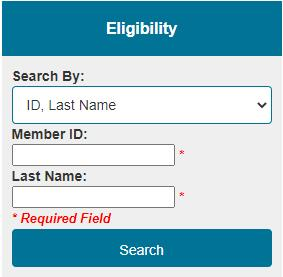
Revised medical policies
Two medical policies have been posted to allwayshealthpartners.org with 6/1/2021 effective dates. Please go HERE to see the updated policies.
The table below is a brief summary of the policies and the changes.
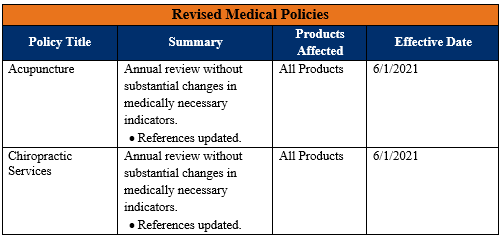
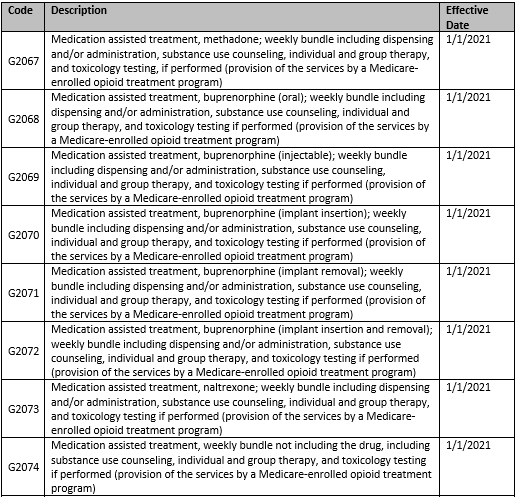
Code Updates
CPT Code Updates
As a reminder to our network the following service are not covered across all lines of business:
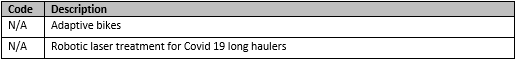
The following service is not covered for My Care Family Plans:
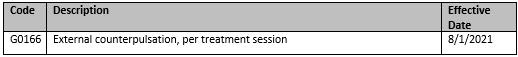
The following services will not be reimbursable for Commercial and ASO Plans:
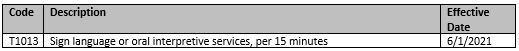
The following service will not be reimbursable for My Care Family Plans:
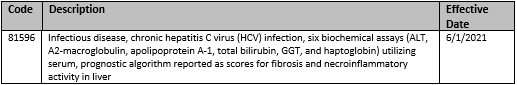
We indicated in the May Newsletter that CPT code 81596 will no longer require a prior authorization effective 6/1/2021. This information is being updated to indicate that code 81596 will still require prior authorization for Commercial and ASO Plans. This has been updated in the May Newsletter.
As a reminder to our network, the following services previously redirect to Optum will not be covered: