- Home
- Provider Administrative newsletter
- New in 2024 - Member ID Cards, Optum Rx, and Complete Access EPO
New in 2024 - Member ID Cards, Optum Rx, and Complete Access EPO
Featured story: Comparing coverage: What's the difference between an HMO, PPO, and EPO?

There are many acronyms used in health insurance that define different plan selections. For example, you’ve probably heard of an HMO or PPO — and maybe even an EPO. So, how do you know which plan to choose? Continue reading to learn about the differences between these plans and which option may work best for you and your health needs. Read the full article.
In this issue:
- Reminder - New member ID cards and numbers for January 1, 2024
- Optum Rx is our new pharmacy benefit manager
- Referral requirements for MGB ACO
- Commercial rate adjustment for telehealth services provided by non-PCP providers beginning January 1, 2024
- Updated Primary Care Sub-Capitation Resource Guide for 2024
- Annual Code and Rate Updates
- Step therapy exception request reminders
- Recall alert - Select batches of Nutramigen Hypoallergenic Infant Formula Powder
- Update - InterQual for Providers
- Complete Access Exclusive Provider Organization (EPO)
- Response to ED Boarding Crisis
- Ensure your information is accurate in the National Plan and Provider Enumeration System (NPPES)
- View Provider manuals in the provider resource center
- Quarterly hospital utilization report
- Medical policy updates
- Medicare provider notification
- Drug code and code updates
- Formulary updates
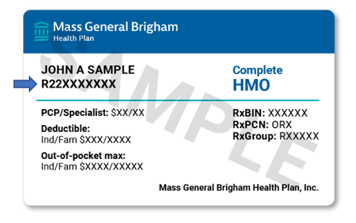
Reminder - New member ID cards and numbers for January 1, 2024
Mass General Brigham Health Plan is updating member ID numbers and cards for all members effective January 1, 2024. Members received a letter with their new ID card. With this update, all individuals across membership populations have the same prefix, R22, in their new ID numbers. There will be a transition period of at least 90 days where both the old and new ID numbers can be used post January 1, 2024.
Frequently asked questions
- Who is receiving new member ID numbers?
All current and new members will be receiving a new member ID number and member ID card. Please note: New members or members with updated eligibility segments will be assigned an R22 member ID number prior to January 1, 2024. Claims should be submitted with the appropriate ID number displaying in the Provider Portal.
- How do I verify a member’s ID number?
Please verify a member’s ID number by visiting the Provider Portal.
- When should members begin using their new member ID numbers?
Members should begin using their new member ID numbers beginning on January 1, 2024.
Please note: if a member receives their R22 ID number before January 1, 2024 due to a change in eligibility, they should begin using that new ID number immediately.
- Which member ID number should I use for services delivered before January 1, 2024?
Please use the current ID number found in the Provider Portal. There will be a transition period of at least 90 days where both the old and new ID numbers can be used post January 1, 2024.
- Will member ID numbers be updated for existing prior authorizations?
Yes, member ID numbers will automatically update for existing prior authorizations.
- If all member IDs start with the same prefix, R22, how do I distinguish the type of membership a patient has?
Please reference our authorization guidelines and/or code checker in the Provider Portal to determine membership type.
- Are benefits changing for members?
No, member benefits are not changing, unless the group and/or member has renewed into a new plan during the same time.
- Will members need to sign up for the Member Portal again?
No, access to the Member Portal will not be impacted.
We ask that you please confirm the ID numbers of all Mass General Brigham Health Plan members when delivering care to ensure that services are properly billed. If members have questions, please direct them to our Customer Service team at 866-414-5533 or HealthPlanCustomerService-Members@mgb.org for additional support.
Optum Rx is our new pharmacy benefit manager
As previously announced, Optum Rx is Mass General Brigham Health Plan's new pharmacy benefit manager (PBM) effective January 1, 2024. As health care changes at a rapid pace, Mass General Brigham Health Plan continues to innovate and build on our total cost of care model. To create lasting value for our clients and members we serve now and, in the future, we changed our pharmacy vendor to Optum Rx. Making pharmacy care more affordable, accessible, supportive, and personal for our members is a shared goal with Optum Rx.
For frequently asked questions (FAQs) about Optum Rx and Specialty Fusions, please visit our dedicated provider resource page.
Referral requirements for Mass General Brigham ACO
Mass General Brigham ACO referral requirements will not change in 2024. A recent announcement from MassHealth stated a change in its referral requirements beginning January 2024 for members enrolled in a Primary Care ACO. Mass General Brigham ACO is an MH Accountable Care Partnership Plan (ACPP) and is not impacted by this change.
Commercial rate adjustment for telehealth services provided by non-PCP providers beginning January 1, 2024
At the beginning of the COVID-19 pandemic, we implemented a temporary change to reimburse telehealth services on parity with in-person visits, in alignment with public health emergency recommendations and regulatory guidance.
On January 1, 2024, we returned to the pre-pandemic practice of a rate differential for services rendered through telehealth versus in-person. Services delivered via telehealth will pay at 85% of in-person rates, with exceptions for primary care and behavioral health. Primary Care services will continue to be reimbursed at 100% of in-person rates. Our behavioral health network is managed by Optum Behavioral Health. Optum BH applies rate parity for services delivered via telehealth. The MA DPH establishes rates for Early Intervention and Early Intensive Behavioral Intervention.
As we return to pre-pandemic operations and policies, we make these changes in accordance with MA 211 CMR 52.00, which implements MA Chapter 260 of the Acts of 2020 and related guidance. We will continue to communicate with you as more information becomes available.
Updated Primary Care Sub-Capitation Resource Guide for 2024
MassHealth has made changes to the Primary Care Sub-Capitation Program effective January 1, 2024. MassHealth has updated the list of included and excluded specialists. View the updated guide.
Annual Code and Rate Updates
Mass General Brigham Health Plan reviews its fee schedules quarterly, to ensure that they are current, comprehensive, and consistent with industry standards, to the extent supported by its systems. In most cases, changes involve adding fees for new or existing codes to supplement the fees already on the fee schedule.
Consistent with prior years, Mass General Brigham Health Plan will update its Commercial/PPO physician, ambulance, drug, DME, laboratory, radiology, and outpatient hospital fee schedules to incorporate new codes, effective January 1, 2024. Rate updates to existing CPT and HCPCS codes will occur on July 1, 2024.
With a few exceptions, Mass General Brigham Health Plan will continue to base fees on the Centers for Medicare & Medicaid Services (CMS) and MassHealth fee schedules, adjusted to achieve the contracted level of reimbursement.
Commercial/PPO Physician Fee Schedules
- Mass General Brigham Health Plan will continue to base physician reimbursement on CMS RVU’s.
- Mass General Brigham Health Plan will continue to base drug, vaccine, and toxoid reimbursement on CMS Part B levels, as indicated on the CMS Part B drug quarterly notices. If no CMS pricing is available, drug pricing will be set in relation to average wholesale price (AWP). Reimbursement for vaccines and toxoids will continue to be updated on a quarterly basis.
- Consistent with prior years, reimbursement will be based on a combination of outpatient, ancillary, and surgical fee schedules.
- Mass General Brigham Health Plan will continue to base drug, vaccine, and toxoid reimbursement on CMS Part B levels, as indicated on the CMS Part B drug quarterly notices. If no CMS pricing is available, drug pricing will be set in relation to average wholesale price (AWP). Reimbursement for vaccines and toxoids will continue to be updated on a quarterly basis.
-
- Mass General Brigham Health Plan will continue to base physician reimbursement on MassHealth published rates.
- Consistent with prior years, Mass General Brigham Health Plan will update its Medicaid physician, ambulance, drug, DME, laboratory, radiology, and outpatient hospital fee schedules to incorporate new codes, effective January 1, 2024. Rate updates to existing CPT and HCPCS codes will occur within 30 days of receipt of notification of rate changes from MassHealth.
Medicare Advantage Fee Schedules
- Mass General Brigham Health Plan will update its Medicare Advantage inpatient, outpatient, ancillary and professional fee schedules/pricers to incorporate new codes and update rates, effective January 1, 2024.
Step therapy exception request reminders
Massachusetts step therapy law, effective October 1, 2023, contains broad reforms to step therapy protocols for Medicaid and commercial carriers, including new step therapy exception criteria. Providers can submit a step therapy exception request as part of the electronic prior authorization form, if applicable.
Mass General Brigham Health Plan applauds and appreciates the state’s efforts to increase access to healthcare and treatment through the new step therapy law. Having worked closely with the state to enhance access to medically necessary medications, we look forward to additional clarifying guidance from the state as we use permitted step therapy measures to keep care affordable for our members.
Here's what providers need to know:
You can request a step therapy exception if you have evidence to believe the lower step treatments are not clinically appropriate, based on one or more of the following criteria:
You can request a step therapy exception if you have evidence to believe the lower step treatments are not clinically appropriate, based on one or more of the following criteria:
1. Member has previous history of one or more of the following:
o Failure on the lower step therapy
o Failure on another therapy in the same pharmacologic class or with the same mechanism of action as the lower step therapy
o Stability on a prescription of the higher step treatment
2. The lower step therapy is not clinically appropriate because it is:
• Contraindicated
• Likely to cause an adverse reaction
• Likely to cause physical/mental harm
• Is expected to be ineffective based on known characteristics
- Step therapy exception requests and appeals will be reviewed and granted or denied within 3 business days following the receipt of all necessary information.
- If additional delay would result in significant risk to the health or well-being of the patient, urgent requests can be submitted for review within 24 hours following the receipt of all necessary information.
- Please provide clinical notes (e.g., name and strength of failed alternative and description of failure) references from peer reviewed journals, etc. during submission of step therapy exception requests and/or appeals.
- Our updated step therapy exception criteria can be found here: Commercial, MassHealth. Please ensure all required documentation is submitted.
- Medical necessity criteria are still required where applicable.
- Please continue to ensure timely submission of prior authorization requests for both pharmaceutical and infusion medications. Prior authorizations for pharmacy should be submitted to Optum Rx (contact information below)
|
Medical and Specialty Medications All Plans: |
Phone: 877-519-1908 |
Fax: 855-540-3693 |
|
Non-Specialty Medications All Plans |
Phone: 800-711-4555 |
Fax: 844-403-1029 |
- For infused medications, please submit prior authorizations via our provider portal.
Recall Alert - Select Batches of Nutramigen Hypoallergenic Infant Formula Powder
The FDA has announced that Reckitt/Mead Johnson Nutrition has voluntarily recalled select batches of Nutramigen Hypoallergenic Infant Formula Powder due to a possible bacterial contamination.
Consumers who have Nutramigen Hypoallergenic Infant Formula Powder with batch codes below should stop using it and throw it away or contact Reckitt/Mead Johnson Nutrition (contact info below) for a refund:
- ZL3FHG (12.6 oz cans)
- ZL3FMH (12.6 oz cans)
- ZL3FPE (12.6 oz cans)
- ZL3FQD (12.6 oz cans)
- ZL3FRW (19.8 oz cans)
- ZL3FXJ (12.6 oz cans)
The products have a UPC Code of 300871239418 or 300871239456 and “Use By Date” of 1 Jan 2025. No other U.S. distributed Nutramigen batches or other Reckitt products are impacted, according to the FDA.
If consumers have any questions, they can contact Reckitt/ Johnson Mead Nutrition at 866-534-9986 24/7 or by email at consumer.relations@rb.com.
Update - InterQual for Providers
Mass General Brigham Health Plan will be updating their InterQual to the October 2023 Release on February 5, 2024.
Complete Access Exclusive Provider Organization (EPO)
We are constantly expanding our plan offerings to meet the healthcare needs of our customers and your patients. To support this goal, Mass General Brigham Health Plan will introduce our Complete Access Exclusive Provider Organization (EPO) plan in 2024. For additional information and FAQs, please visit Complete Access EPO for providers
Response to ED Boarding Crisis
Mass General Brigham Health Plan complies with regulatory guidance to ensure Hospitals are reimbursed for behavioral health crisis evaluations and stabilization services provided in the Emergency Department in response to the ED Boarding crisis.
This applies to:
- Commercial members, for dates of service 11/01/2022 and forward per MA DOI Bulletin 2022-08.
- Medicaid members, for dates of service 01/03/2023 through 09/30/2023, per Mass Health guidance including MCE Bulletin 93 published November 2022.
- Medicaid members, for dates of service 10/01/2023 and forward, per the MA Inpatient Acute General RFA effective 10/01/2023.
Mass General Brigham Health Plan complies with regulatory guidance to ensure Hospitals are reimbursed for behavioral health crisis evaluations and stabilization services, crisis management, recovery support navigators and the initiation of medication treatment for Opioid Use Disorders in the ED per the MA Inpatient Acute General RFA effective 10/01/2023.
Provider payment guidelines | Mass General Brigham Health Plan
Ensure your information is accurate in the National Plan and Provider Enumeration System (NPPES)
According to the Centers for Medicare and Medicaid Services (CMS), it is essential for providers to keep their profile in the National Plan and Provider Enumeration System (NPPES) accurate and up-to-date..
Please visit the NPPES site at https://nppes.cms.hhs.gov to ensure the following information is accurate:
- Phone number
- Address
- Clinical practice/group name
- Plans accepted
How to update your profile:
- Visit the NPPES site at https://nppes.cms.hhs.gov.
- Select the “Magnifying Glass” ICON to View the desired National Provider Identifier (NPI) application.
- Select the “Pencil” ICON to Edit the desired NPI application
- Access the page that contains the information to be updated by selecting the ‘Next’ button located at the bottom of each page or by selecting the desired page from the left hand navigation bar.
- Update the necessary information.
- Once all desired information is updated navigate to the Submission page. Check the Certification Statement box at the bottom of this page.
- Select Submit. This button will not be enabled until you check the Certification Statement box at the bottom of this page.
If you experience any difficulty accessing the NPPES, please contact the NPI Enumerator at 1-800-465-3203 or customerservice@npienumerator.com.
2024 ConnectorCare changes
New in 2024, Mass General Brigham Health Plan will be offering our full network product, Complete HMO in ConnectorCare to meet the new Massachusetts Health Connector’s requirement. The Complete HMO will be sold alongside our current high-performance network product, Select HMO. Click here to see a sample of the Complete HMO ConnectorCare member ID card.
View Provider manuals in the provider resource center
We’ve made it easy for you to do business with Mass General Brigham Health Plan by organizing popular forms and resources on one resource page. In the provider resource center, you will find provider manuals for Commercial, ACO, and Medicare Advantage plans.
The Provider Manual includes important information on how you can support your patient. Topics in the Provider Manual include:
- Quality Improvement Program
- Utilization Management Decision-Making - This includes information regarding our decision-making process and procedures. We do not specifically reward practitioners or other individuals conducting utilization review for issuing denials of coverage or service, nor do we provide financial incentives to UM decision-makers to encourage decisions that result in under-utilization.
- Credentialing and Re-credentialing Processes
- Member Rights & Responsibilities
- Practitioner Rights & Responsibilities
- Interpreter Services
View provider manuals in the Provider resource center
Hospital inpatient utilization report
The latest quarterly hospital inpatient utilization report is now available. To review this report, click on the Reports tab in the Provider Portal and select Clinical Reports. If you do not have access to the Provider Portal, you may register here.
Medical policy updates
Eight (8) medical policies were reviewed and passed by the Mass General Brigham Health Plan’s Medical Policy Committee. These policies are now posted to MassGeneralBrighamHealthPlan.org. The table below is a summary.
For more information or to download our medical policies, go to https://www.massgeneralbrighamhealthplan.org/providers/medical-policies and select the policy under the medical policy listings.
|
Medical Policies |
|||
|
Policy Title |
Summary |
Products Affected |
Effective Date |
|
Assisted Reproductive Services/Infertility Services
|
March 2024: Off-cycle Review. The following changes were made: · On Page 3: General Eligibility Criteria o Added 2c o Redefined and clarified the language around the specific causes of infertility by adding 2d. I, II, III. o Under Ovarian Reserve Assessment criteria, added language to specify that time in which AMH testing needs to be done as seen in 3b. III. o Age limit applied to item 3c. · On Page 4 under Subheading Artificial Insemination (AI)/Intrauterine Insemination (IUI), added clarifying language for members <44 years of age. · On Page 5 Under IVF Coverage Criteria o language regarding infertility definition, tubal factor and endometriosis reordered to prior section. o Removed requirement on six cycle limit of IVF o Under Frozen Embryo Transfer (FET) language reordered, clarified and added 1. 2. and 3. · On Page 6 under Donor Egg Services for Infertility; language reordered and clarified without substantive changes to criteria. · On Page 7 Under ICSI, added language “Partner has had urology consultation” to #1 · On Page 9 under Individuals with a Sterilization Reversal section; added the following language to 1b. “and there have been no ectopic pregnancies since the reversal”. |
Commercial and Medicare plans |
3/1/2024 |
| Medicare Advantage Administrative Guidelines |
January 2024. Annual Update. Administrative changes made to the coverage guidelines section. Added language regarding Medical Policy Committee. Intent unchanged. Changes made to Table 1 to reflect updated hyperlinks. High-tech radiology section removed. References updated. |
Medicare Advantage |
1/1/2024 |
|
Breast Surgeries |
January 2024: Annual Review. Medicare Advantage added to table. Medicare Variation added. Codes updated. References updated. |
All products |
1/1/2024 |
|
Reconstructive and Cosmetic Procedures |
January 2024: Annual Review. Added criteria for Otoplasty. Added Bracing to the Pectus Carinatum criteria. Updated codes. |
All products |
1/1/2024 |
|
HIV-Associated Lipodystrophy Syndrome |
January 2024: Annual Review. Medicare Advantage added to table 1. Medicare Variation language added. References updated. |
All products |
1/1/2024 |
|
Phototherapy and Photochemotherapy for Dermatologic Conditions |
January 2024: Annual Update. On page 1 under UVB Photochemotherapy, added Mycosis fungoides, Sezary Syndrome next to CTCL. References updated. |
All products |
1/1/2024 |
|
UVB Home Phototherapy Units for Skin Disease |
January 2024: Annual Update. References updated. |
Commercial and Medicare plans |
1/1/2024 |
|
Balloon Dilation of the Eustachian Tube [NEW POLICY] |
February 2024: Effective Date. A procedure for members 18 years of age and older with chronic eustachian tube dysfunction. |
Commercial and Medicare plans |
2/1/2024 |
2024 Medicare provider notification
View the Medicare Provider Notification here.
Drug code and code updates
View code updates for January 2024 here.
Formulary and NCCN update
View the formulary updates here.