- Home
- Provider Administrative newsletter
- Annual updates to fee schedules, telemedicine modifier requirements, and resources that meet members on their gender affirmation journey in June 2022
Annual updates to fee schedules, telemedicine modifier requirements, and resources that meet members on their gender affirmation journey in June 2022
Featured story: Resources that meet members on their gender affirmation journey
At AllWays Health Partners, we want our members to live their healthiest life in alliance with our commitment to diversity, equity, and inclusion. That’s why we offer gender-affirming care management for members in need of help navigating healthcare, answers to questions, or support along their gender journey. Continue reading to learn more about our gender affirmation care management program available to members of AllWays Health Partners.
In this issue:
- Telemedicine modifier requirements
- Annual updates to physician and outpatient fee schedules
- Medical policy updates
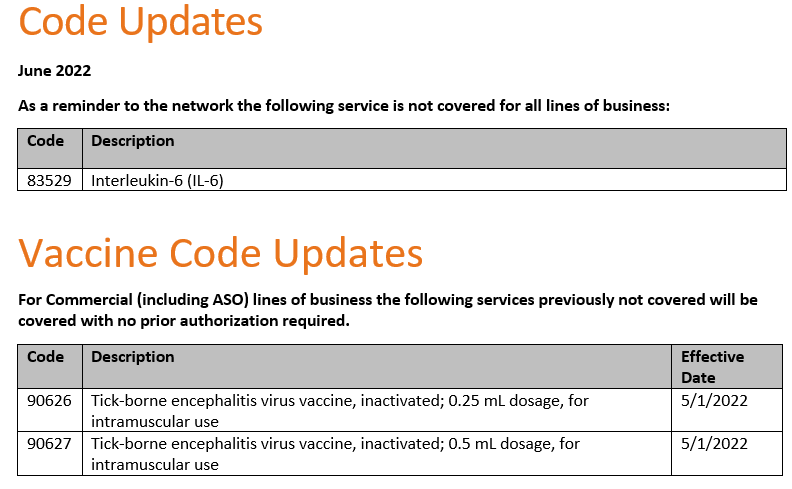
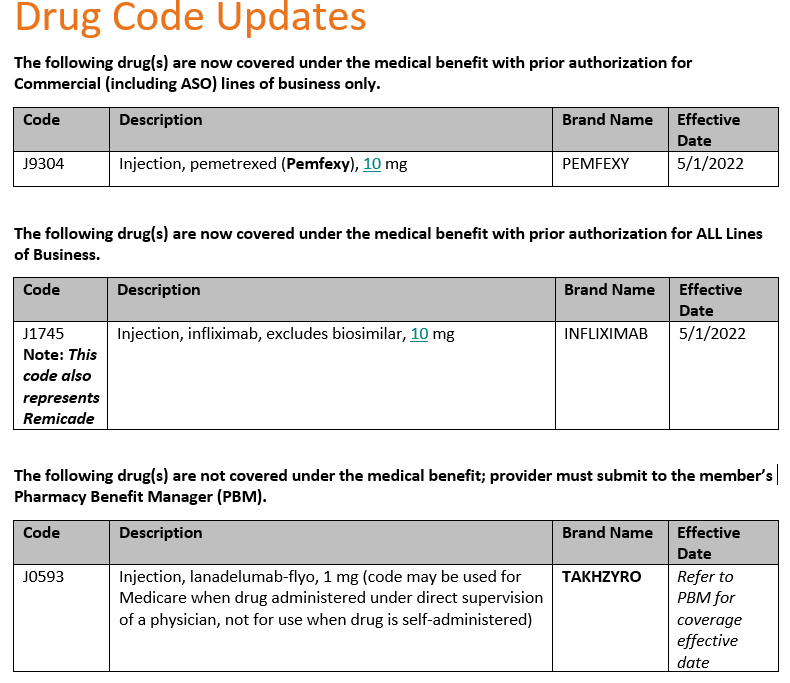
- Code updates
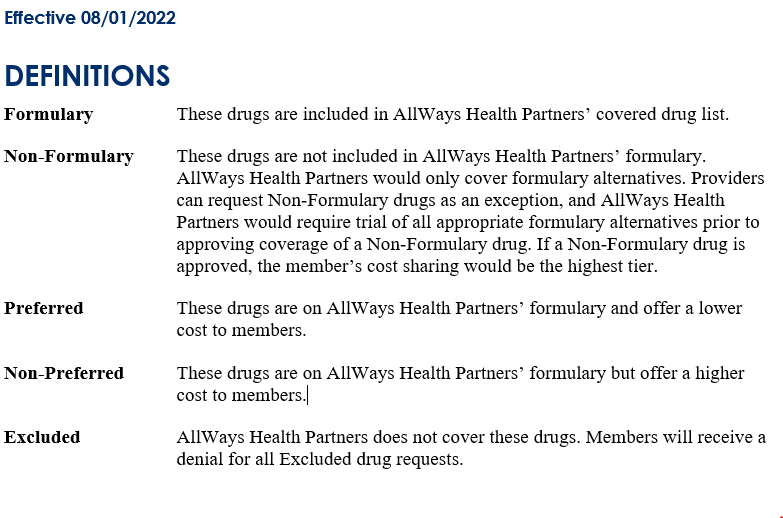
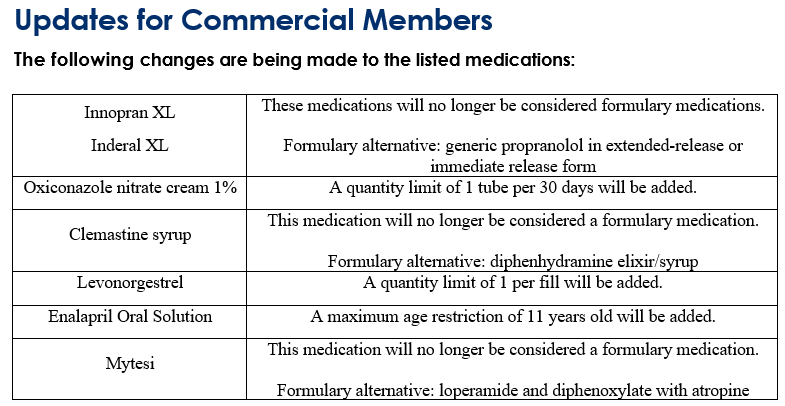
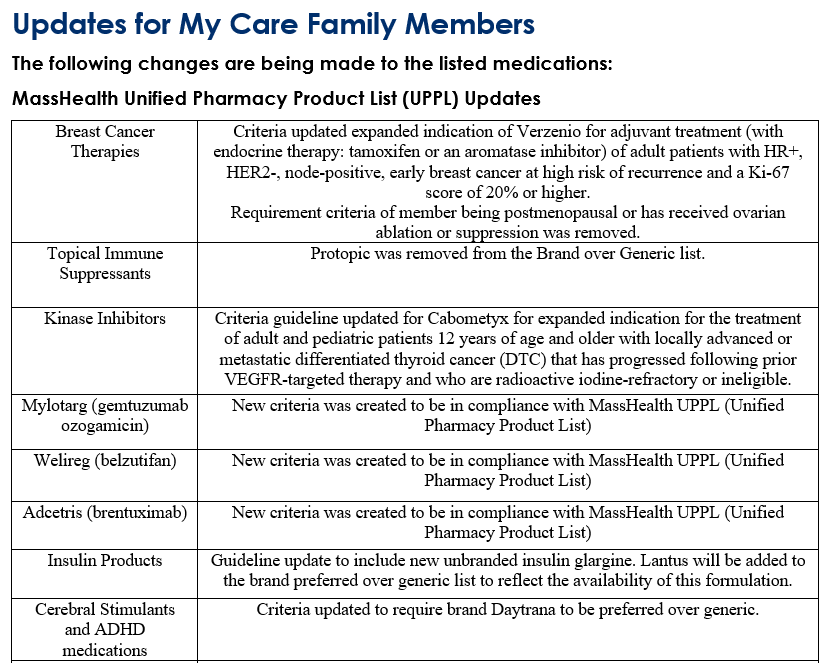
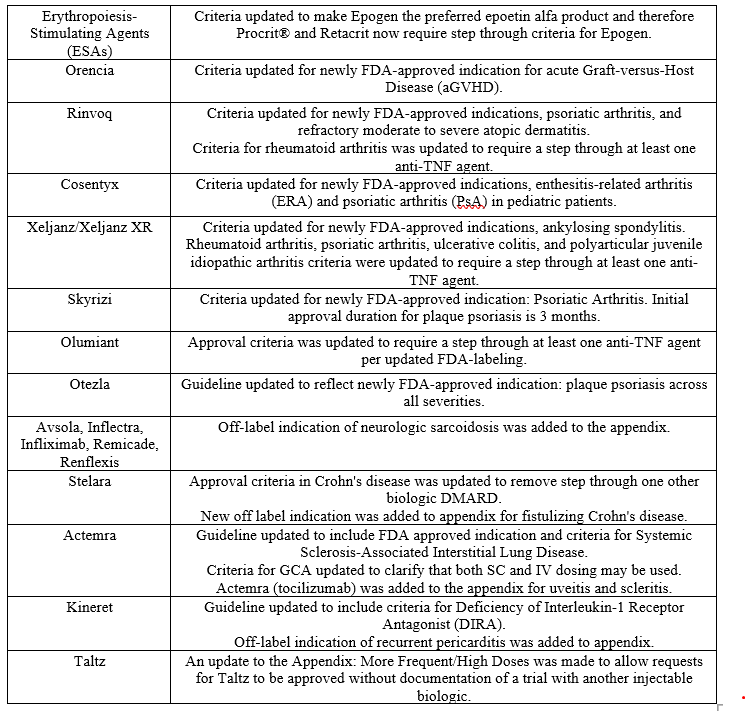
- Formulary updates
Telemedicine modifier requirements
As a reminder, AllWays Health Partners requires telemedicine modifiers when billing for in-person services provided via telemedicine.
- Effective for dates of service beginning August 1, 2022, professional claims must be submitted with POS 02 (Telehealth provided other than in patient’s home) or 10 (Telehealth provided in patient’s home) and the appropriate modifier below, to indicate the type of modality. Claims that are submitted without one of the following modifiers will deny:
- Modifier 95 (Synchronous Telemedicine Service Rendered via a Real-Time Interactive Audio and Video Telecommunications System)
- Modifier V3 (Via audio-only telehealth)
- Modifier GQ (Via asynchronous telecommunications system)
- Facility claims should be submitted with the appropriate revenue code(s), CPT/HCPCS code(s) and modifier GT (Via interactive audio and video telecommunication systems) for telemedicine services. Claims with dates of service beginning August 1, 2022 submitted without this modifier will deny.
Note: Telephonic and Digital E/M’s should not be appended with telemedicine modifiers.
Annual updates to physician and outpatient fee schedules
AllWays Health Partners reviews its physician and outpatient fee schedules quarterly, to ensure that they are current, comprehensive, and consistent with industry standards, to the extent supported by its systems. In most cases, changes involve adding fees for new or existing codes to supplement the fees already on the fee schedule.
Consistent with prior years, AllWays Health Partners updated its Commercial/PPO physician, ambulance, drug, DME, laboratory, radiology and outpatient hospital fee schedules to incorporate new codes, effective January 1, 2022. With a few exceptions, AllWays Health Partners will continue to base fees on the Centers for Medicare & Medicaid Services (CMS) and MassHealth fee schedules, adjusted to achieve the contracted level of reimbursement.
Commercial/PPO Physician Fee Schedules
• Rate updates to existing CPT and HCPCS codes will occur on July 1, 2022.
• AllWays Health Partners will continue to base physician reimbursement on CMS RVU’s & anesthesia conversion factor.
• AllWays Health Partners will continue to base drug, vaccine and toxoid reimbursement on CMS Part B levels, as indicated on the CMS Part B drug quarterly notices. If no CMS pricing is available, drug pricing will be set in relation to average wholesale price (AWP). Reimbursement for vaccines and toxoids will continue to be updated on a quarterly basis.
• AllWays Health Partners will continue to base DME reimbursement on the CMS DME POS/PEN fee schedules.
Commercial/PPO Outpatient Fee Schedules
• Consistent with prior years, reimbursement will be based on a combination of outpatient, ancillary and surgical fee schedules.
• AllWays Health Partners will continue to base drug, vaccine and toxoid reimbursement on CMS Part B levels, as indicated on the CMS Part B drug quarterly notices. If no CMS pricing is available, drug pricing will be set in relation to average wholesale price (AWP). Reimbursement for vaccines and toxoids will continue to be updated on a quarterly basis.
• AllWays Health Partners will continue to base DME reimbursement on the CMS DME POS/PEN fee schedules.
My Care Family Fee Schedules
• AllWays Health Partners will continue to base physician reimbursement on MassHealth published rates, where published rates exist.
• Consistent with prior years, AllWays Health Partners updated its Medicaid physician, ambulance, drug, DME, laboratory, radiology and outpatient hospital fee schedules to incorporate new codes, effective January 1, 2022. Rate updates to existing CPT and HCPCS codes will occur within 30 days of receipt of notification of rate change from MassHealth.
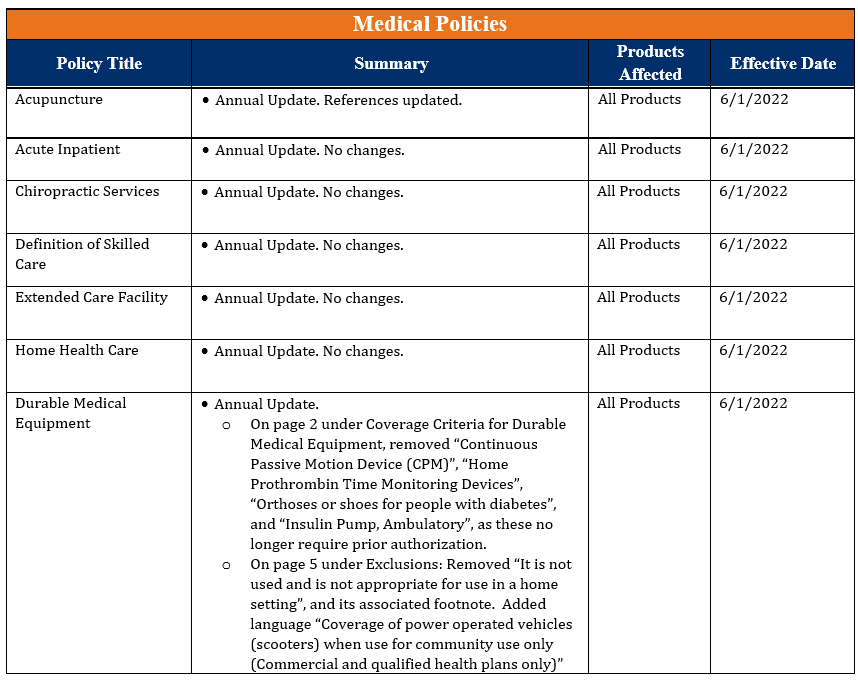
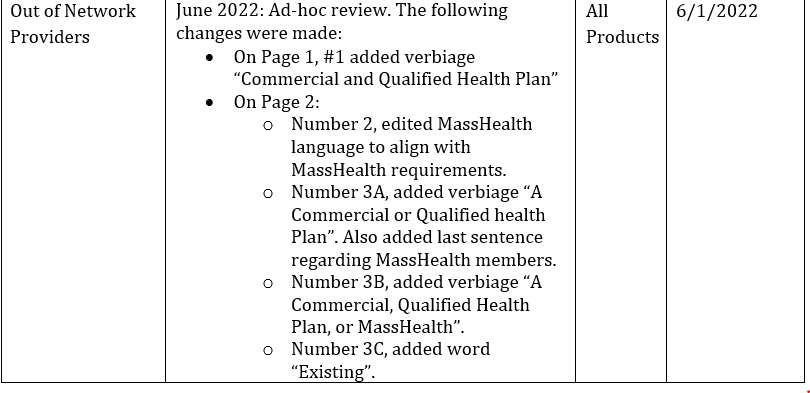
Medical policy updates
Seven medical policies were reviewed and passed by the AllWays Health Partners Medical Policy Committee. These policies are now posted to allwayshealthpartners.org The table below is a summary of the policies and the changes.
For more information or to download our medical policies, go to https://www.allwayshealthpartners.org/providers/medical-policies and select the policy under the medical policy listings.