New in 2024: Complete Access EPO
Check back frequently for the latest updates.
About the plan
We are constantly expanding our plan offerings to meet the healthcare needs of our customers and your patients. To support this goal, Mass General Brigham Health Plan introduced our Complete Access Exclusive Provider Organization (EPO) plan in 2024.
If you've received a notice from Mass General Brigham Health Plan indicating that you will be in the Complete Access EPO Plan network, there is no additional action required for you to start seeing members in 2024.
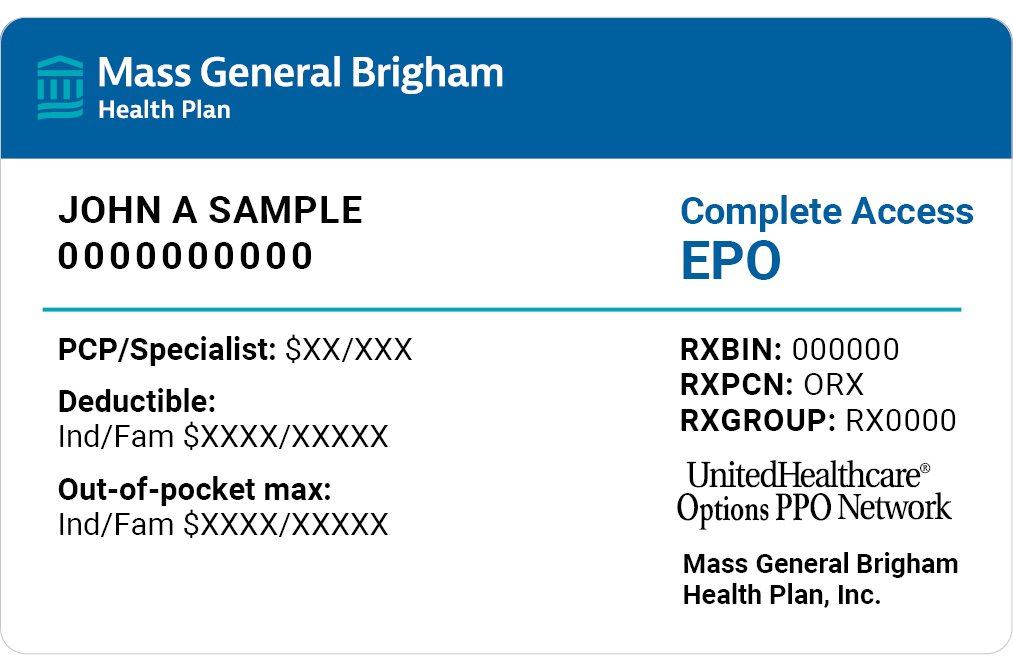
Member ID cards
Frequently asked questions
Complete Access Exclusive Provider Organization (EPO) is a variation of our Complete HMO plan network.
Members can find additional information on the Member Portal.
Yes, all eligibility can be checked by visiting the Provider Portal.
Reimbursement will be the same as the Complete HMO.
There is no dedicated prefix for the Complete Access EPO plan.
Your existing Commercial contract with Mass General Brigham Health Plan will not change.
You can confirm your participation by utilizing our online provider directory or via the Provider Portal
Standard referral rules apply. You can check referral requirements here.
Authorizations will be required where applicable. For the most up-to-date information, visit our prior authorization guidelines page.
No, if a member is moving from one Commercial plan to the Complete Access EPO Plan any authorization that was previously obtained should be valid.
There is no change for paper claim submission. Providers should refer to the information on our claims page.
The electronic payer ID will remain the same.
We plan to adhere to the current standard filing rules, which is 90 days unless otherwise specified in your contract. Providers should refer to their contracts for any questions.
No, we’ll have one combined EOP for all lines of business.
We're here to help! Please send any additional questions to: CompleteAccessEPOContractingMailbox@mgb.org
Please sign-up for our administrative newsletter communications to get the latest information sent right to your inbox.
Never miss an update
Be the first to get the latest news, tips, and information when you subscribe to our provider Administrative Newsletter.